1. Patient Information:
- Gender: Male
- Age: 70
- Diagnosis: Squamous cell carcinoma of the right lung
2. Medical History:
The patient experienced chest tightness, shortness of breath, cough, and sputum production without obvious cause in March 2024, occasionally accompanied by chest pain and blood-streaked sputum. In May 2024, the patient visited the outpatient clinic of the First Affiliated Hospital of the Air Force Medical University for evaluation. A chest CT revealed multiple space-occupying lesions in the right lung, suspected to be malignant, with mediastinal lymph node metastasis. A lung biopsy was performed, and the pathological results (Pathology No. B202416110) indicated squamous cell carcinoma in the upper right lung.
Immunohistochemistry (IHC) Results:
- Positive markers: Ki-67 (~30%), INI-1(+), SMARCA4(+), p40(+), CK5/6(+), p63(+)
- Negative markers: TTF-1(-), NapsinA(-), INSM1(-), p16(-), NUT(-)
- PD-L1 (SP263) TPS ≈1%
The diagnosis of malignant tumor in the upper lobe of the right lung was confirmed. The patient and family sought further treatment and visited our hospital on May 23, 2024. A PET/CT scan showed:
1. An irregular soft tissue mass in the posterior segment of the right upper lobe with increased metabolism, highly suggestive of right lung cancer.
2. A small nodule in the right middle lobe with increased metabolism, and multiple small and enlarged lymph nodes in the mediastinum and around the superior vena cava, also with increased metabolism, suggesting metastasis.
3. Small and slightly enlarged lymph nodes in the left neck (Level IV) and left clavicular region with increased metabolism, possibly metastatic.
Based on the imaging findings and the 9th edition AJCC staging criteria, the patient was staged as cT4N3M0 IIIC (AJCC 9th). After a multidisciplinary team (MDT) discussion and exclusion of contraindications, the patient began carbon ion therapy on June 11, 2024, targeting the intrapulmonary metastasis and mediastinal lymph node metastasis. The treatment plan included:
- PTV T PRO: 56 Gy (RBE) in 14 fractions, 4 Gy (RBE) per fraction
- PTV V+: 16 Gy (RBE) in 4 fractions, 4 Gy (RBE) per fraction
- PTV nd PRO: 48 Gy (RBE) in 12 fractions, 4 Gy (RBE) per fraction
- PTV nd V: 64 Gy (RBE) in 16 fractions, 4 Gy (RBE) per fraction
- PTV T: 72 Gy (RBE) in 18 fractions, 4 Gy (RBE) per fraction
Concurrently, the patient received one cycle of EP chemotherapy starting on May 28, 2024:
- Etoposide (50 mg/m²): 0.8 g IV on days 1-5 and 29-33
- Cisplatin (50 mg/m²): 80 mg IV on days 1, 8, 29, and 36
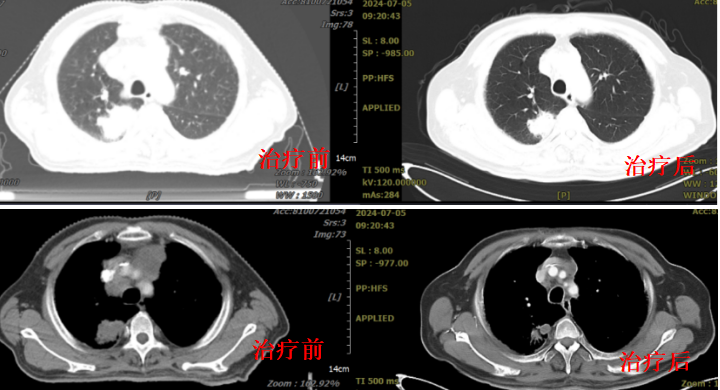
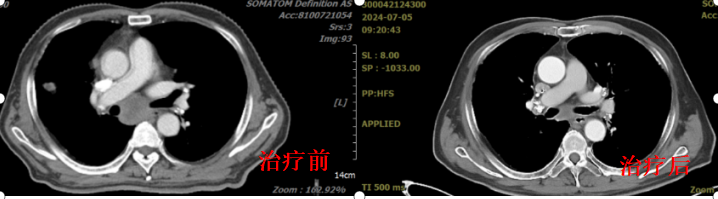
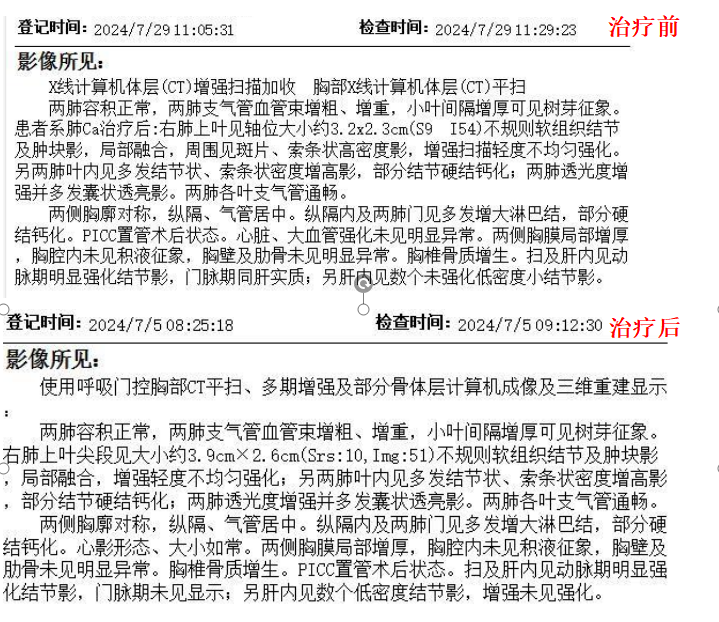
The combined chemoradiotherapy was well-tolerated. A follow-up chest CT showed that the lesion in the apical segment of the right upper lobe had decreased from 44.0 × 37.6 × 50.2 mm to 3.9 × 2.6 cm, with a 22.3% reduction in the longest diameter, indicating a good response. The patient was discharged with improvement.
One month after carbon ion therapy, a follow-up examination at our hospital revealed a mass in the right upper lobe with surrounding inflammation, which had further decreased in size compared to the previous scan (July 5, 2024), measuring approximately 3.2 × 2.3 cm. The tumor in the right upper lobe had shrunk by 37% compared to pre-treatment, achieving a partial response (PR) in efficacy evaluation.
3. Treatment options:
Carbon Ion Therapy for Intrapulmonary Metastasis and Mediastinal Lymph Node Metastasis of Right Lung Cancer:
- PTV T PRO: Total dose 56 Gy (RBE) in 14 fractions, 4 Gy (RBE) per fraction
- PTV V+: Total dose 16 Gy (RBE) in 4 fractions, 4 Gy (RBE) per fraction
- PTV nd PRO: Total dose 48 Gy (RBE) in 12 fractions, 4 Gy (RBE) per fraction
- PTV nd V: Total dose 64 Gy (RBE) in 16 fractions, 4 Gy (RBE) per fraction
- PTV T: Total dose 72 Gy (RBE) in 18 fractions, 4 Gy (RBE) per fraction
Concurrent Chemotherapy with EP Regimen:
- Etoposide (50 mg/m²): 0.8 g IV infusion on days 1-5 and 29-33
- Cisplatin (50 mg/m²): 80 mg IV infusion on days 1, 8, 29, and 36
4. Therapeutic Effect: