A Beacon of Hope: Heavy Ion Radiotherapy for Malignant Thymoma (Case Report)
Patient Ren XX, female, 56 years old.
Chief complaint: More than 6 years after thymoma surgery.
Past medical history: Previously healthy, currently able to take care of herself independently.
Admission date: January 7, 2025
Diagnosis: Malignant thymoma (Type B1, Masaoka-Koga Stage IV)
Current medical history: The patient found a mediastinal tumor during a physical examination on July 5, 2018. Thus, she visited Beijing Cancer Hospital on July 13, 2018. A chest CT showed a space-occupying lesion of 4.7×3.2 cm in the left anterior mediastinum, but no treatment was given at that time. Later, the patient occasionally felt back pain, but had no chest pain, chest tightness, dysphagia, or limb weakness. On July 19, 2018, she visited Shanghai Pulmonary Hospital. On July 20, 2018, the chest CT report showed: A soft tissue mass shadow in the left anterior mediastinum, possibly a malignant lesion, and further examination was recommended; left pleural metastasis could not be excluded. On July 20, 2018, the chest MRI report showed: A space-occupying lesion in the left upper mediastinum, considered to be a thymoma; nodular lesions in the left pleura, considered to be metastases. On July 23, 2018, PET-CT showed: From the head to the upper third of the thigh: 1. A soft tissue mass in the left anterior mediastinum with increased FDG metabolism, suggesting a high possibility of a malignant lesion originating from the thymus, and pathological clarification was recommended. 2. A spindle-shaped nodular shadow in the left pleura (at the level of the 10th posterior rib) with increased FDG metabolism, considered to be a metastatic lesion. The diagnosis was clear: Mediastinal tumor, c-Masaoka-Koga stage: III. On July 23, 2018, under general anesthesia, she underwent "total thymectomy + resection of chest wall nodules". The postoperative pathology (B18-11553) showed: (Mediastinum) Thymoma, Type B1, with a size of 7×6×4.5 cm. The tumor invaded the surrounding adipose tissue (>3 mm), the "left upper lobe" and the "left mediastinal pleura"; tumor tissue was visible beside the "left phrenic nerve"; the sent "pleural nodules" and "posterior rib diaphragmatic nodules" were tumor tissue. The postoperative recovery was good. She underwent left pleural radiotherapy in August 2018, DT: 13 Gy/13 F (4 fields), 100 cGy/F. Then she had regular reexaminations, and the condition was stable. On December 2024, a re-examination by CT showed abnormally enhanced nodules in the anterosuperior mediastinum, and tumor recurrence was considered. Now the patient and her family came to our hospital for further treatment. She was admitted to the outpatient department with the diagnosis of "malignant thymoma". Since the onset of the disease, the patient has been clear-minded, in a good mental state, with normal diet, poor sleep, normal urination and defecation, and no obvious weight loss.
Admission and Treatment
After admission, relevant examinations were completed. After excluding contraindications, radical carbon ion radiotherapy for recurrent thymoma was initiated on January 15, 2025. The radiotherapy doses were as follows: For the part of the left pleura far from the stomach and colon, 72 Gy (RBE)/18 Fx was administered; for the lesions adjacent to the heart border and esophagus, 52 Gy (RBE)/13 Fx was administered; for the part of the left pleura close to the stomach and colon, a basic dose of 40 Gy (RBE)/10 Fx was administered.
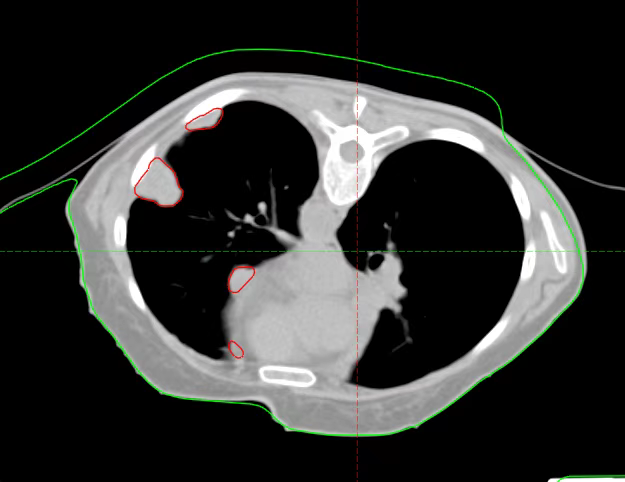
Before Radical Regional Treatment
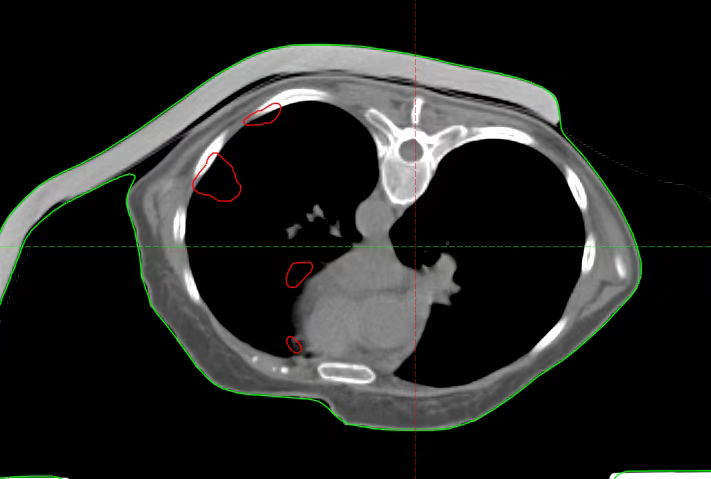
After Radical Regional Treatment
After the completion of pre-radical regional treatment, the lesions in the radical treatment area significantly regressed. Due to the maximum tolerated dose limitations of the stomach and intestines, the lesions near the stomach and colon in the left pleura did not receive the radical treatment dose. After a multidisciplinary consultation at our hospital, combined with the actual situation of the patient and previous treatment experience, it was decided to adopt the technique of intraoperatively placing gauze pads to isolate vital organs, which was first initiated by our hospital. The departments of surgery, anesthesiology, ICU, radiotherapy physics, radiotherapy technology, imaging, carbon ion operation and maintenance personnel, and ambulance transfer personnel cooperated actively. After the surgeon placed gauze pads to isolate the stomach and colon during the operation, the ICU and anesthesiologist accompanied the patient to the radiotherapy center. The radiotherapy technicians made a positioning mold, and the imaging department performed a positioning CT scan. After the positioning scan, the patient was transferred to the ICU for close observation. The radiotherapist completed the target area delineation work, and then the physics room developed a radiotherapy plan for the patient. After the plan was completed, it was verified together with the technicians and operation and maintenance personnel, and at the same time, the physician completed the pre-radiotherapy repositioning verification. After the verification was correct, the patient received a single high-dose radical radiotherapy. After the radiotherapy was completed, the patient was transferred back to the operating room to remove the gauze pad. The whole process involved the cooperation of multiple departments. Under the command of the hospital leadership, each part was carried out in an orderly manner, and the intraoperative radiotherapy was accurately completed in the shortest time. After the operation, the patient's vital signs were stable and there were no special discomforts.
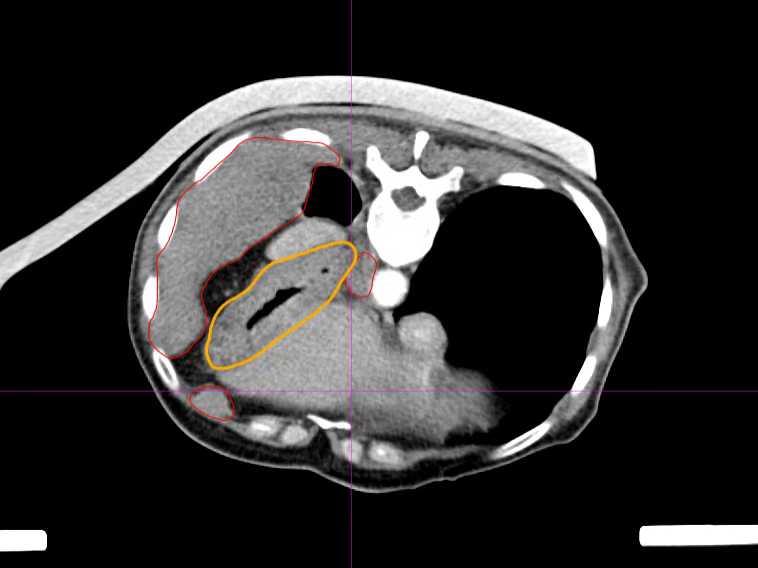
The relationship between the lesion and the stomach before placing the gauze pad (red indicates the lesion, yellow indicates the stomach)
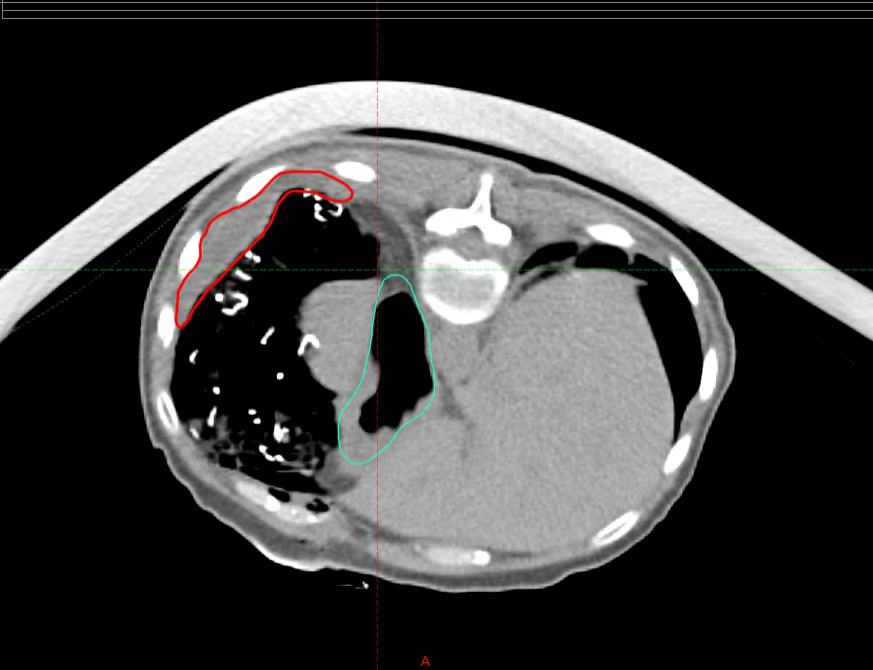
The relationship between the lesion and the stomach after placing the gauze pad (red indicates the lesion, blue indicates the stomach)
