Male patient, aged 66, admitted to the hospital due to a "confirmed diagnosis of right lung adenocar
Medical History:
The patient, a 55-year-old male with a history of hypertension for over 7 years, has been treated with Nifedipine GITS for blood pressure control, which has been stable. On June 11, 2019, following a "cold," the patient experienced cough and expectoration. A chest CT at Sir Run Run Shaw Hospital of Zhejiang University revealed a nodule in the right upper lobe of the lung (33mm×36mm), with invasion of the anterior segment bronchus of the right upper lobe and compression of the superior vena cava. Bronchoscopy and biopsy indicated adenocarcinoma of the right lung. The lung cancer driver gene test was negative; PD-L1: TPS 20%. Starting from July 15, 2019, the patient underwent four cycles of regular chemotherapy with the "Pemetrexed + Nedaplatin" regimen at Xinjiang Occupational Disease Hospital, with an efficacy evaluation of SD. A PET/CT in July 2020 showed a hypermetabolic soft tissue mass in the right upper lobe of the lung (44mm×37mm, SUVmax 20.4), suggesting malignant tumor of the right lung, with nodular thickening with hypermetabolism on the right pleural side (SUVmax 6.2), considered pleural metastasis. Due to tumor progression, the patient underwent three cycles of combined chemotherapy with "Pemetrexed + Nedaplatin + Camrelizumab," achieving a PR evaluation after chemotherapy. Due to grade III gastrointestinal adverse reactions, chemotherapy was discontinued, followed by four cycles of monotherapy with "Camrelizumab" immunotherapy. A chest CT review at the Third People's Hospital of Xinjiang Uyghur Autonomous Region on March 19, 2021, indicated a lobulated soft tissue mass beside the mediastinum in the right upper lobe of the lung, with the lesion protruding into the mediastinum, considered lung cancer, slightly enlarged compared to the film from February 20, 2021. In April 2021, a PET-CT at our hospital showed a soft tissue density nodule with increased metabolism beside the bronchus of the right upper lobe, mostly considered lung cancer; several small nodules with increased metabolism in the local right pleural area, mostly considered metastasis; and a crescent-shaped high-density nodule with increased metabolism in the right parietal lobe, with possible metastasis. A plain scan and enhanced MR of the head on December 15, 2022, showed a nodular lesion beside the posterior horn of the right lateral ventricle, with surrounding extensive edema signals, considered metastasis with hemorrhage based on the patient's history.
Examinations:
Imaging Examinations: A chest CT at Sir Run Run Shaw Hospital of Zhejiang University in June 2019 revealed a nodule in the right upper lobe of the lung (33mm×36mm), with invasion of the anterior segment bronchus of the right upper lobe and compression of the superior vena cava. Bronchoscopy and biopsy indicated adenocarcinoma of the right lung. Gene testing: EGFR/ALK/ROS1/RAS/BRAF/MET/NTRK(-). PD-L1: TPS 20%. A PET-CT at the Affiliated Tumor Hospital of Xinjiang Medical University in July 2020 showed a hypermetabolic soft tissue mass in the right upper lobe of the lung (44mm×37mm, SUVmax 20.4), considered malignant tumor of the right lung, with nodular thickening with hypermetabolism on the right pleural side (SUVmax 6.2), considered pleural metastasis. A PET-CT at our hospital in April 2021 indicated stenosis and truncation of the anterior segment bronchus of the right upper lobe, with a soft tissue density nodule with increased metabolism beside the upper lobe bronchus, mostly considered lung cancer; several small nodules with increased metabolism in the local right pleural area, mostly considered metastasis; and a crescent-shaped high-density nodule with increased metabolism in the right parietal lobe, with possible metastasis. An MRI of the head on December 15, 2022, showed a nodular lesion beside the posterior horn of the right lateral ventricle, with surrounding extensive edema signals, considered metastasis with hemorrhage based on the patient's history.
Treatment Plan:
After discussion by the hospital's MDT, the treatment plan was determined as follows: Carbon ion therapy for right lung cancer, right pleural metastatic cancer, and brain metastatic cancer, followed by sequential immune checkpoint inhibitor therapy.
Therapeutic effect:
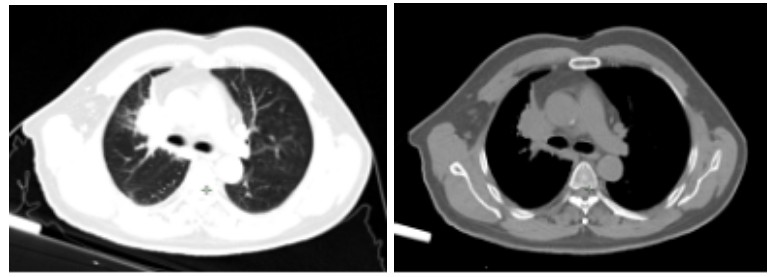
Figure 1.Chest tumor before carbon ion therapy
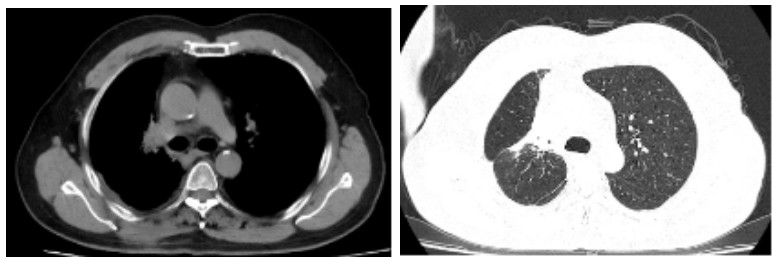
Figure 2. One year after carbon ion therapy for chest tumor
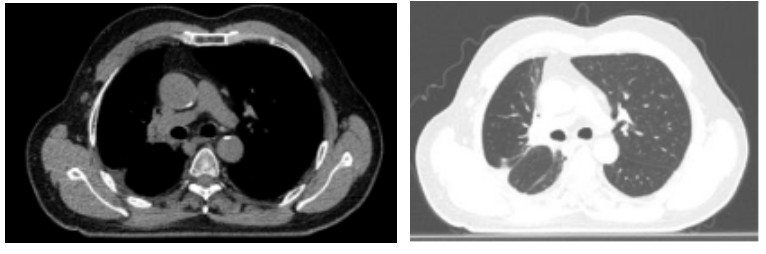
Figure 3. Two years after carbon ion therapy for chest tumor
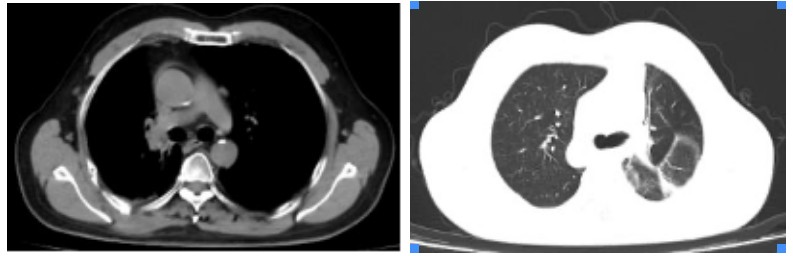
Figure 4. Three years after carbon ion therapy for chest tumor
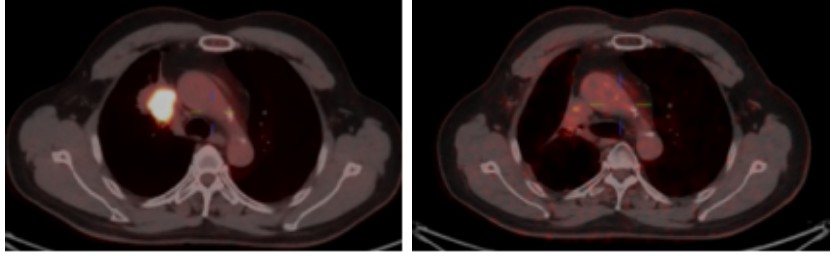
Figure 5. Comparison of the primary pulmonary lesions on PET/CT before and 2 years after heavy ion therapy
