Female patient, 51 years old, right lung adenocarcinoma
【Typical Case】 Complete Tumor Disappearance 4 Years After Carbon Ion Therapy for Right Lung Adenocarcinoma
History Description
Female patient, 51 years old. Chest CT on May 25, 2021, revealed an irregular lobulated soft tissue mass in the anterior basal segment of the right lower lobe, suggestive of peripheral lung cancer; multiple enlarged lymph nodes in the mediastinum and hilar regions, possibly metastatic. PET-CT on June 4, 2021, showed a space-occupying lesion in the basal segment of the right lower lobe and multiple enlarged mediastinal lymph nodes with increased glucose metabolism, indicating mediastinal lymph node metastasis. Bronchoscopic biopsy on June 10, 2021, confirmed poorly differentiated carcinoma in the anterior basal segment of the right lower lobe, suggestive of lung adenocarcinoma. Genetic testing revealed an EGFR exon 21 L858R mutation. The physician recommended oral "osimertinib" therapy.
Treatment Course
On July 9, 2021, the patient was admitted to our hospital and underwent 21 sessions of carbon ion radiotherapy for right lung cancer, combined with oral "osimertinib" targeted therapy. Post-treatment chest CT indicated a partial response (PR). Follow-up PET-CT on January 9, 2023, revealed patchy shadows adjacent to the right lower lobe bronchus with corresponding bronchial and bronchiolar narrowing/occlusion, accompanied by mildly increased local metabolism. Findings suggested post-therapy suppression or disappearance of active lesions, local inflammation, and focal atelectasis. Scattered dense lymph nodes in the mediastinum and bilateral hilar regions showed no abnormal metabolism. Overall, the efficacy was evaluated as complete response (CR) after carbon ion radiotherapy and targeted therapy.
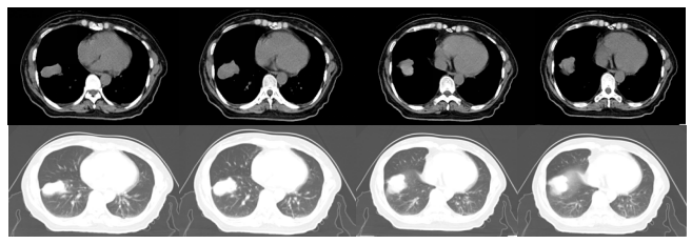
Figure 1: Chest CT (June 21, 2021): Irregular lobulated soft tissue mass in the anterior basal segment of the right lower lobe, suggestive of peripheral lung cancer; multiple enlarged lymph nodes in the mediastinum and hilar regions, possibly metastatic.
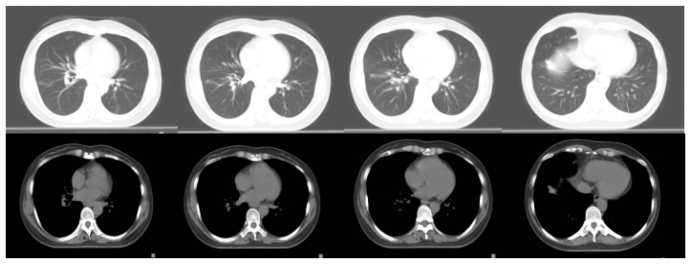
Figure 2: Follow-up chest CT (August 9, 2021): Abnormal density in the anterior basal segment of the right lower lobe with adjacent obstructive pneumonia; multiple small nodules and partial fibrosis in both lungs and subpleural regions.
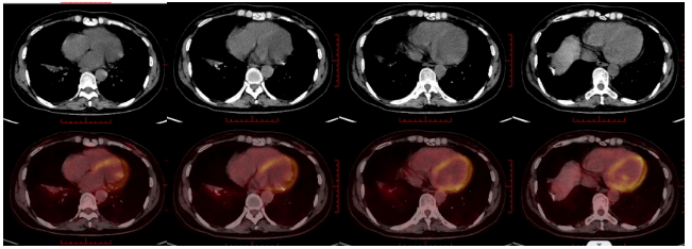
Figure 3: Follow-up PET-CT (17 months post-treatment, January 9, 2023):
① Patchy shadows adjacent to the right lower lobe bronchus with corresponding bronchial/bronchiolar narrowing/occlusion and mildly increased local metabolism, suggesting post-therapy suppression or disappearance of active lesions, local inflammation, and focal atelectasis.
② Scattered dense lymph nodes in the mediastinum and bilateral hilar regions without abnormal metabolism.
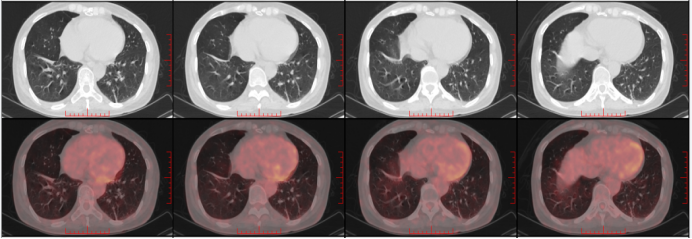
Figure 4: Follow-up PET-CT (4 years post-treatment, August 7, 2025):
① Patchy increased density in the right lower lobe without abnormal metabolism, slightly reduced metabolism compared to prior, suggesting post-therapy suppression of activity, local atelectasis, or inflammation.
② Scattered fibrotic small lymph nodes in the mediastinum and bilateral hilar regions with mild metabolism, likely inflammatory. Streaky increased density in the right upper lobe with air bronchogram and no abnormal metabolism, suggestive of inflammation; tiny nodule in the right middle lobe without abnormal metabolism, likely inflammatory.
Expert Perspective
Lung cancer is mainly divided into non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). Pulmonary adenocarcinoma and squamous cell carcinoma belong to NSCLC, while SCLC accounts for a smaller proportion (≈15%). Pulmonary adenocarcinoma, squamous cell carcinoma, and SCLC are the three most common types. Pulmonary adenocarcinoma is the most prevalent, comprising 35%–40% of all lung cancers. It is typically centrally located, grows relatively slowly, and has lower metastatic potential. It commonly affects non-smoking women and younger individuals (often aged 40–50). Prognosis for pulmonary adenocarcinoma is better than for SCLC or squamous cell carcinoma. Subtypes include adenocarcinoma in situ (AIS), minimally invasive adenocarcinoma (MIA), and invasive adenocarcinoma. AIS has no peripheral invasion and a 5-year survival rate of 100%. MIA exhibits ≤5 mm invasion with near-100% 5-year survival. Early-stage invasive adenocarcinoma achieves >80% 5-year survival.
Treatment begins with genetic testing, as 40%–50% of non-smoking female patients harbor driver mutations. Targeted therapy (e.g., osimertinib for EGFR mutations) is highly effective if mutations are present. For mutation-negative cases, immunotherapy or chemotherapy is indicated. Platinum-based doublet chemotherapy (e.g., pemetrexed + platinum) is particularly effective for pulmonary adenocarcinoma.
For stage I NSCLC treated with heavy ion therapy:
- Miyamoto et al. reported 90% 5-year local control and 68% 5-year survival in 79 patients.
- Shioyama et al. (306 patients across 4 Japanese institutions) reported 83.6% 3-year overall survival, 69.4% progression-free survival, and 88.6% local control.
For stage II–III NSCLC with heavy ion therapy:
- Karube et al. (64 patients across 3 centers) reported 62.2% 2-year overall survival, 42.3% progression-free survival, and 81.8% local control.
- Hayashi et al. (32 patients aged >80) reported 83.5% 2-year local control, 46.7% progression-free survival, and 68.0% overall survival.
In contrast, conventional photon radiotherapy (RTOG 9410 trial) for stage III NSCLC (610 patients) yielded a median survival of 15.6 months and 13% 5-year survival with concurrent chemoradiation.
Heavy ion radiotherapy represents a major breakthrough in precision oncology for pulmonary adenocarcinoma. Its core value lies in achieving biologically potent tumor eradication through ultra-precise physical dose delivery, offering a curative option for inoperable patients. With technological advancements and protocol optimization, it holds promise as a first-line treatment for early and locally advanced pulmonary adenocarcinoma.
