Unveiling the Secrets: Day Surgery vs. Traditional Surgery for Great Saphenous Vein Varicose
Unveiling the Secrets: Day Surgery vs. Traditional Surgery for Great Saphenous Vein Varicose
Great saphenous vein varicose is a common vascular condition, and after diagnosis, many patients face choices regarding their surgical management. Leveraging an advanced day surgery management model, the Department of Orthopedics and Soft Tissue Surgery at Wuwei Cancer Hospital has successfully enabled patients with this condition to complete all treatment and be discharged safely within 24–48 hours of admission.
This highly efficient approach carries profound significance. For patients, it dramatically shortens hospital stays, allowing them to quickly resume their normal daily routines. Following surgery, patients go home to recuperate the next day—saving several days compared to traditional inpatient models. Meanwhile, significantly reduced hospitalization costs effectively ease financial burdens: these savings make timely treatment accessible to more patients who might otherwise face delays.
Next, we’ll take a detailed look at the key features of the two approaches—day surgery and traditional surgery—to help patients make more informed decisions.

Surgical Duration and Procedure
Traditional Surgery
Traditional great saphenous vein varicose surgery typically requires a longer duration to complete the entire workflow. Prior to the procedure, patients usually need to be admitted to the hospital 1–3 days in advance. Upon admission, they undergo a series of comprehensive examinations—including a complete blood count (CBC), coagulation function tests, liver and kidney function assessments, electrocardiogram (ECG), and lower extremity vascular ultrasound—to evaluate their overall physical status and rule out any surgical contraindications.
One day before surgery, nurses perform preoperative skin preparation (commonly known as "hair removal") and guide patients through bowel preparation (e.g., fasting and water restriction) to minimize the risk of intraoperative infection.
On the day of surgery, the patient is wheeled into the operating room. Once anesthesia takes effect, the surgeon proceeds with conventional techniques: multiple incisions are made in the leg to sequentially ligate and strip the main trunk of the great saphenous vein and its varicose branches. The operation typically lasts 1–2 hours.
Postoperatively, the patient is transferred back to the ward and requires prolonged bed rest—absolute immobility is mandatory for the first 24 hours, after which they gradually resume activity.

Day Surgery
The day surgery workflow is even more streamlined and efficient. Patients typically undergo necessary preoperative tests—such as a complete blood count (CBC), coagulation function tests, electrocardiogram (ECG), and lower extremity vascular ultrasound—1–2 days before surgery to confirm eligibility for the day surgery model.
On the surgery day, after completing preoperative preparations, patients are wheeled into the operating room. Day surgery primarily uses minimally invasive techniques; the Department of Orthopedics and Soft Tissue Surgery at Wuwei Cancer Hospital employs microwave ablation combined with sclerotherapy, a less invasive and relatively simpler approach. The procedure usually takes around 30 minutes, enabling the surgery to be performed with "zero" incisions.
Postoperatively, patients are observed in the post-anesthesia care unit (PACU) briefly. Once anesthesia has worn off and vital signs are stable, they return to the ward. After a short observation period, if there is no significant discomfort and patients meet discharge criteria, they can be discharged on the same day or the next day.

2.Length of Hospital Stay and Recovery Time
Traditional Surgery
Traditional surgery involves a longer hospital stay, typically lasting 5–7 days or even longer. Postoperatively, patients require close observation and care in the hospital, including wound dressing changes, infection prophylaxis, and monitoring of lower extremity blood circulation. During hospitalization, their activity is restricted, and they must follow doctors’ and nurses’ guidance for rehabilitation exercises.
After discharge, patients still need time to recover—generally, it is recommended to rest for 2–4 weeks before gradually returning to normal work and life. Throughout recovery, they must avoid prolonged standing or walking to prevent wound dehiscence or recurrence of varicose veins.
Day Surgery
One of the biggest advantages of day surgery is its short hospital stay: patients usually go home on the same day or the next day after the procedure. While the hospitalization is brief, this does not mean recovery is accelerated—however, because day surgery primarily uses minimally invasive techniques with less trauma, patients tend to recover faster postoperatively.
Generally, after a short rest at home, patients can resume basic daily activities. During recovery, they must follow their doctor’s instructions: wear medical compression stockings, engage in appropriate movement, promote lower extremity blood circulation, and speed up healing.

Risk of Complications
Traditional Surgery
Traditional surgery, due to multiple incisions and greater tissue trauma, carries a relatively higher risk of postoperative complications. Common issues include wound infection, bleeding, hematoma formation, deep venous thrombosis (DVT) of the lower extremities, and nerve injury.
•Wound infection may delay healing, requiring antibiotic treatment;
•Bleeding or hematoma formation may necessitate reoperation for hemostasis or hematoma evacuation;
•If a lower extremity DVT dislodges, it can trigger a pulmonary embolism (PE)—a life-threatening complication;
•Nerve injury may lead to sensory abnormalities (e.g., numbness) or motor dysfunction (e.g., weakness) in the affected leg.

Day Surgery
Day surgery primarily uses minimally invasive techniques, causing less tissue trauma and carrying a relatively lower risk of postoperative complications. However, it is not entirely complication-free: procedures like laser ablation, radiofrequency ablation, or microwave ablation may lead to issues such as skin burns or phlebitis; similarly, sclerotherapy can result in local pain, hyperpigmentation, or thrombophlebitis.
That said, these complications have a relatively low incidence, and most are mild—resolving with appropriate management.
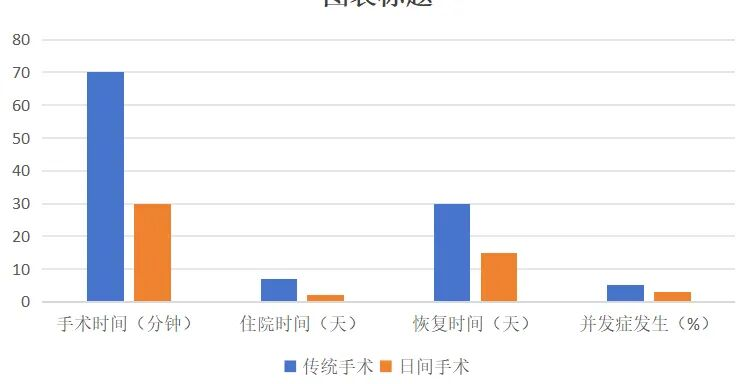
In summary, both day surgery and traditional surgery for great saphenous vein varicose have their respective advantages and disadvantages. Day surgery offers shorter operation time, shorter hospital stays, faster recovery, lower costs, and relatively lower complication risks—but it demands certain physical fitness from patients and specific post-operative care. Traditional surgery, though associated with longer operation/hospital stays, higher costs, and slightly elevated complication risks, may still be a more reliable choice for patients with complex conditions or severe varicose veins.
When selecting a surgical approach, patients should fully communicate with their doctors and weigh factors like their own condition, physical status, and financial capacity to make the most informed decision tailored to themselves.
The Department of Orthopedics and Soft Tissue Surgery at Wuwei Cancer Hospital has accumulated extensive experience in the daytime management of varicose vein surgery. This expertise is expected to help the hospital take solid strides toward enhancing medical service efficiency.

Ye Kui
Deputy Chief Physician
Specialty: Vascular Surgery
Clinic Locations:
•Consultation Room 710, 7th Floor, Outpatient Department, Central Campus
•1st Floor, Outpatient Building; 2nd Floor, No. 7 Surgical Building, Heavy Ion Campus
Contact: +86-13642116650
Professional Background:
Graduated from Tianjin Medical University with a PhD degree. Has been engaged in vascular medicine for 15 years, completing fellowship training at Tianjin Nankai Hospital. Proficient in minimally invasive treatment of great saphenous vein varicose, skilled in minimally invasive sclerotherapy for varicose veins, and experienced in interventional surgery for lower extremity arteriosclerosis obliterans. Has rich expertise in the application of devices including stents, drug-eluting balloons (DEBs), shockwave balloons, guide wires, and catheters.
Proficient in standardized anticoagulation for deep venous thrombosis (DVT), scientific comprehensive management, determining indications for inferior vena cava filter (IVCF) placement, interventional surgery for pulmonary embolism (PE), IVCF implantation and retrieval, dialysis access creation and maintenance, comprehensive treatment of diabetic foot, and performing amputations. Expertise in early diagnosis and treatment of visceral artery diseases (e.g., renal artery stenosis, subclavian artery stenosis, superior mesenteric artery (SMA) stenosis or thromboembolism) to prevent systemic inflammatory response.
Has a strong grasp of aortic diseases and can perform endovascular treatment. Capable of interventional hemostasis for visceral organs and open surgical repair for arterial injury or embolism. Skilled in interventional placement of biliary/intestinal stents, jejunostomy feeding tubes, and intestinal obstruction catheters.
Passionate about research, having successfully completed a Tianjin Municipal Health Commission Science and Technology Project and achieved official result registration.
Department of Bone and Soft Tissue Surgery, Wuwei Cancer Hospital, Gansu Province
Wuwei Cancer Hospital, Gansu Province, is the first specialized hospital for bone and soft tissue tumors in the province. After 20 years of continuous development, the Department of Bone and Soft Tissue Surgery has established a comprehensive diagnostic and treatment system centered on bone and soft tissue tumors while covering other subspecialties. Through ongoing technical advancement, the department has achieved significant growth. It houses the Comprehensive Bone Metastasis Treatment Center and Minimally Invasive Spine Treatment Center, with inpatient wards located on the 1st floor (Ward 1) and 2nd floor (Ward 2) of Building 7 in the Heavy Ion Campus. The department has 90 beds, featuring elegant wards and a robust technical team.
Clinical Services & Technologies
The department offers a wide range of cutting-edge treatments:
•Intra-articular PRP Injection for Osteoarthritis: Platelet-rich plasma (PRP) injections deliver proven efficacy for mild-to-moderate osteoarthritis.
•Mesenchymal Stem Cell Therapy: Clinical trials of mesenchymal stem cell injections show promising results for rheumatic immune diseases and osteoarthritis.
•Routine Joint Replacements: Hip, knee, ankle, shoulder, elbow, and wrist replacements to restore function in degenerative or destructive joint diseases.
•Custom Prosthetic Replacement for Extremity/Pelvic Tumors: Limb-salvage surgery for bone and soft tissue tumors of the extremities.
•Endoscopic Spine Surgery: Treats lumbar disc herniation and spinal stenosis, improving quality of life for patients with degenerative lumbar conditions.
•Endoscopic Examination/Treatment for Large Joints: Minimally invasive evaluation and therapy for hips, knees, ankles, shoulders, elbows, and wrists.
•Microwave Thermal Coagulation & Argon-Helium Cryotherapy: Targets spinal/limb bone metastases to relieve pain and eliminate tumors—combined with vertebroplasty or bone cement injection for enhanced efficacy.
•Standardized Biopsies: Precise sampling for bone and soft tissue tumors across all anatomical sites.
•Tumor Resection + Limb Salvage: Combined with radiotherapy/chemotherapy to boost cure/survival rates and quality of life for bone/soft tissue tumors.
•Spacer Implantation for Heavy Ion Radiotherapy: Protects normal organs during treatment and reduces adverse reactions in adjacent tissues.
•Spinal Tuberculosis Surgery: Anterior, posterior, lateral, and minimally invasive approaches for diverse tuberculosis lesions.
•Fracture Reduction: Surgical realignment for spinal and extremity fractures.
•Vascular Anastomosis: Foundational technique for repairing/reconstructing damaged extremity vessels.
•Arteriovenous Fistula Creation: Long-term vascular access for hemodialysis patients.
•Standardized Extremity Vascular Disease Treatment: Evidence-based care for vascular conditions of the arms/legs.

Preliminary Review: Zhang Jie
Final Review: Ma Shuqian
