The Forgotten Fall: The "Silent Threat" of Chronic Subdural Hematoma in the Elderly
The Forgotten Fall: The "Silent Threat" of Chronic Subdural Hematoma in the Elderly
Chronic subdural hematoma (CSDH) is one of the common diseases in neurosurgery, with an annual incidence of 14-20 cases per 100,000 people. It refers to a hematoma that develops between the dura mater and the arachnoid membrane and is often termed a "silent" cerebral hemorrhage, predominantly affecting the elderly. A characteristic feature of CSDH is that the initial head injury is often minor, with no immediate discomfort after the incident. Clinical symptoms typically appear a long time later, and many patients do not even recall having sustained a head injury. The onset is insidious, and the clinical symptoms and signs are non-specific. Many patients present with memory decline, dizziness, unsteady gait, psychiatric symptoms, or urinary incontinence, which can easily be misdiagnosed as Alzheimer's disease.
With the aging population, the increasing prevalence of cardiovascular and cerebrovascular diseases (such as metabolic syndrome, obesity, diabetes, and cerebral infarction), the use of anticoagulants and antiplatelet medications, and the rising incidence of cerebral atrophy, the rate of CSDH is expected to increase further in the future. CSDH is most common in elderly males (male-to-female ratio 3:1), with the majority of patients being over 65 years old and the average age of onset being 77 years. Most cases occur weeks (≥3 weeks) after a head trauma, though some have no clear history of injury. This trend is projected to continue.

01 Why does CSDH have an "insidious onset" and predominantly affect the elderly?
The reason lies in the phenomenon of cerebral atrophy in the elderly. While the brain undergoes atrophy, the skull size remains unchanged. This creates increased space between the skull and the brain tissue, providing room for a significant amount of blood to accumulate. Because of this extra space, symptoms only begin to appear slowly once the hematoma has grown large enough to exert noticeable pressure on the brain.
When a head injury occurs—even a minor one such as head shaking or jostling from traveling on a bumpy road—the atrophied brain has more room to move within the skull. This increased mobility can stretch and tear the small, fragile bridging veins on the brain's surface or the small veins connected to the dural sinuses, leading to bleeding. This bleeding is typically intermittent and slow. Furthermore, factors in the elderly such as cerebral atrophy, lower intracranial pressure, increased venous tension, or coagulation disorders can prevent the bleeding from stopping, allowing the hematoma to expand gradually until symptoms manifest. This explains why the elderly are the most susceptible population.
02 What are the symptoms?
1.Symptoms of increased intracranial pressure: Headache, vomiting, papilledema.
2.Psychiatric disorders: Dementia, apathy, memory decline, disorientation, and intellectual retardation.
3.Focal neurological symptoms: Hemiplegia, aphasia, numbness, and focal epilepsy.
03 How is it treated?
1.Oral medication: Suitable for cases with minimal bleeding, insignificant symptoms, very advanced age, or patients with surgical contraindications. Some experts recommend oral medications (such as Atorvastatin Calcium, Dexamethasone, etc.) to promote hematoma absorption.
2.Surgical treatment: Surgery is indicated when the hematoma is large, causing significant compression of brain tissue and severe clinical symptoms.
3.Burr hole drainage surgery: A drainage tube is placed into the hematoma cavity during surgery to evacuate as much of the hematoma as possible. The drain is typically removed within 2-3 days after surgery, depending on the drainage output.
4.Craniotomy for hematoma evacuation: This is a more invasive procedure and is not the first-line treatment. It is reserved for cases where closed drainage fails, or when the hematoma contains a large amount of clot or has septations that make burr hole drainage ineffective.
5.Middle meningeal artery (MMA) embolization: This is an interventional procedure. Research has found that the MMA is the primary blood supply to the hematoma membrane, which is a main reason for the hematoma's continued expansion. High-field strength 7T MRI can preoperatively accurately assess the MMA. Embolizing the MMA blocks the blood supply to the hematoma membrane, thereby preventing further enlargement and allowing the body's own clearance mechanisms to absorb the hematoma. This procedure is performed under local anesthesia, has a short duration, and is particularly suitable for elderly patients in poor general health, as it avoids the risks of general anesthesia and endotracheal intubation. As a minimally invasive interventional technique, it causes less trauma, minimal pain, promotes faster patient recovery, shortens hospital stays, and is especially applicable for elderly patients on anticoagulant medication. "Less is more," often leading to better postoperative recovery.
04 Important Notes:
Chronic subdural hematoma (CSDH) is a distinct type of intracranial hemorrhage, different from the common "cerebral hemorrhage" (intracerebral hemorrhage). The bleeding volume can reach 150-200 ml or even more. Its symptoms can mimic acute cerebrovascular diseases. The early symptoms are insidious and non-specific, with a slow progression. If left untreated, the prognosis is poor. However, CSDH is curable with timely treatment, often without leaving neurological deficits (such as headache, hemiplegia, or aphasia).
Elderly individuals, due to mobility issues, are prone to falls leading to head injuries. Furthermore, those taking anticoagulant medications have impaired coagulation, increasing the risk of spontaneous bleeding. Family members must provide careful supervision for the elderly. If a fall occurs, seek medical attention promptly for examination. For anyone who has experienced a head injury, it is crucial to seek immediate medical consultation if symptoms like headache, dizziness, blurred vision, aphasia, or slowed response develop—even three months or longer after the injury.
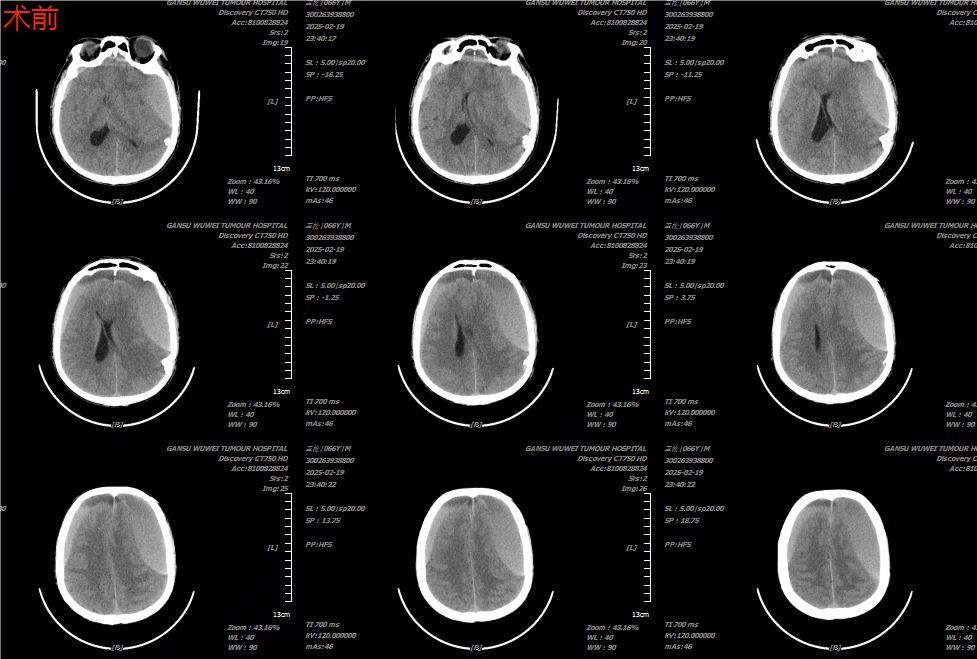
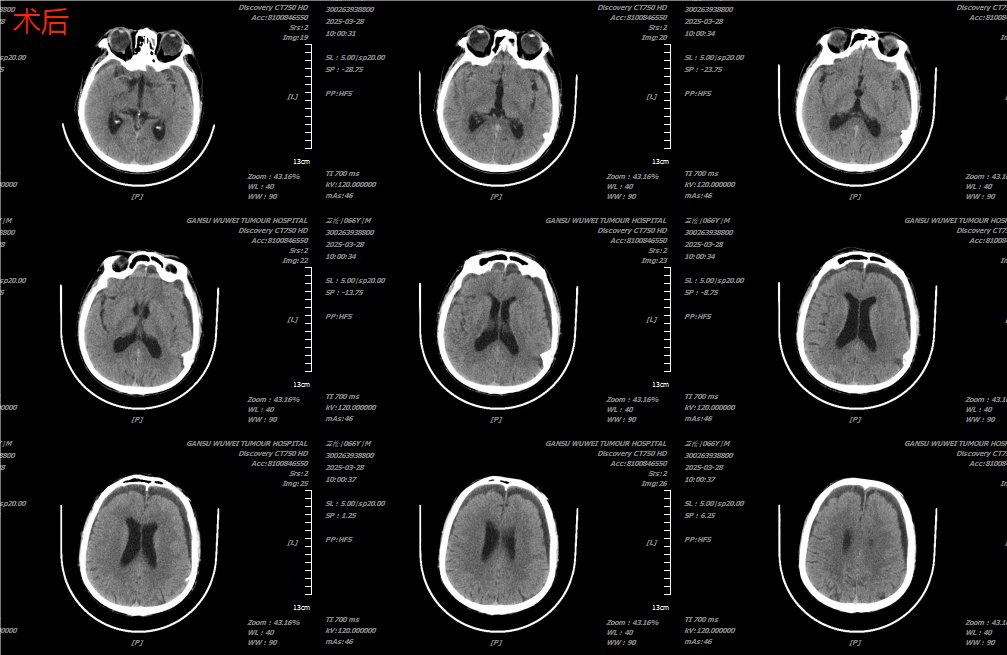
Case Presentation 1
Patient: Male, 66 years old.
Chief Complaint: Headache for over 1 month following trauma, accompanied by sudden syncope and right-sided limb weakness for 5 hours.
Past Medical History: Has a 7-year history of hypertension, with irregular medication adherence (blood pressure control status unknown). Sustained a head injury one month ago. No history of blood transfusion. No known allergies to food or drugs. Denies history of diabetes.
Preliminary Diagnosis: Subdural Hematoma (Bifrontotemporal)
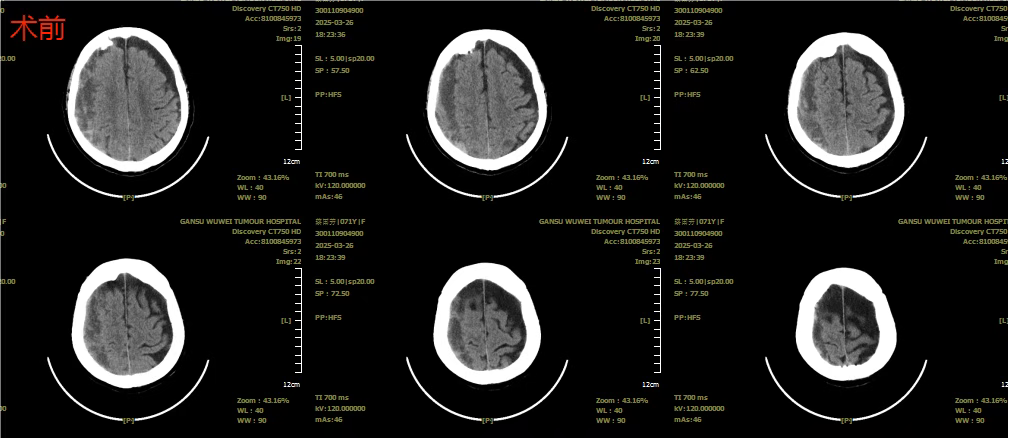
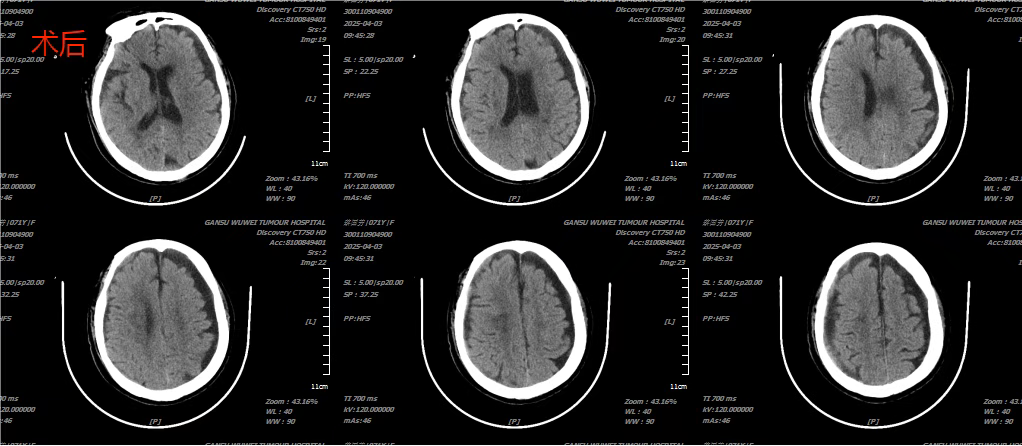
Case Presentation 2
Patient: Female, 71 years old.
Chief Complaint: Weakness in the right lower limb causing walking difficulty for 2 months, worsened over the past 3 days.
Past Medical History:
Hypertension for over 20 years, with highest recorded BP of 180/90 mmHg. Medication regimen includes Valsartan 80mg once daily and Amlodipine Besylate 5mg once daily (current BP control status unknown).
Diabetes Mellitus for over 5 years. Medication regimen includes Metformin Hydrochloride Extended-Release tablets (2 tablets before breakfast, 1 tablet before dinner) and Insulin Aspart (20 units in the morning, 20 units in the evening) for glycemic control.
Underwent cholecystectomy for "gallstones" at another hospital 30 years ago, with postoperative recovery.
Underwent surgical treatment for "left eye cataract" 5 years ago, with postoperative recovery.
Sustained a head injury 3 months ago.
No history of blood transfusion.
No known allergies to food or drugs.
Denies history of diabetes mellitus. (Note: Contradicts the above history; translated as stated.)
Preliminary Diagnosis: Subdural Hematoma (Right Frontotemporoparietal)
Introduction to the Wuwei Medical Science Academy Neuroscience Medical Center
The Neuroscience Medical Center was established through the integration of disciplinary resources from our hospital's Neurosurgery and Neurology departments. It is a key discipline that combines clinical medicine, teaching, scientific research, and talent development. Encompassing multiple specialties including Neurosurgery, Neurology, Neurocritical Care, Neurological Rehabilitation, and Neurointervention, the center provides patients with comprehensive "one-stop" diagnostic and therapeutic services. This integrated approach covers the entire process from disease prevention, diagnosis, and treatment to rehabilitation, psychological support, health education, and long-term follow-up.
The center routinely performs diagnosis and treatment for common neurological conditions such as brain tumors, intracerebral hemorrhage, cerebrovascular malformations, cerebral aneurysms, and traumatic brain injury. The center's capabilities also include interventions for stroke, such as intravenous and intra-arterial thrombolysis, cerebral angiography (via transradial or transfemoral approaches), mechanical thrombectomy, carotid artery stenting, vertebral artery stenting, and interventional embolization of cerebral aneurysms.
The department boasts a rational personnel structure, strong technical capabilities, and extensive medical experience. Our current team includes one permanent expert from the Neurosurgery Department of The First Affiliated Hospital of Lanzhou University, two senior professionals, two mid-level professionals, and two junior-level professionals, three of whom hold master's degrees.
We uphold the developmental philosophy of "integrating humanistic medicine with neuroscience" to build a compassionate and patient-centric medical center. Adhering to a people-oriented approach, we consistently implement our hospital's management principles: "pursuing medical excellence, upholding high moral standards, delivering attentive services, and building a deeply trusted brand." We continue to pioneer innovations and stride forward with confidence.
Preliminary Review: Zhang Jie
Final Review: Ma Shuqian
