Holiday Alert: Preventing Lower Limb Deep Venous Thrombosis
Holiday Alert: Preventing Lower Limb Deep Venous Thrombosis
Holidays are meant to be wonderful stretches of time to relax, recharge, and savor life. Yet during this break, a silent threat has quietly crept up on many—lower extremity deep vein thrombosis (DVT). While most people may not recognize this condition, let’s unpack why it tends to target us during holidays, the risks it poses, and what we can do to prevent and address it.
Ⅰ. Why Is Lower Extremity Deep Vein Thrombosis (DVT) More Likely During Holidays?
(1) Prolonged Immobility of the Lower Limbs
Travel by car or plane: During long-distance trips—whether by automobile or aircraft—cramped quarters limit free movement of the lower legs. Sitting in a fixed position for hours causes leg muscles to relax, disabling their role as the “muscle pump”. This slows venous return from the lower extremities: like a sluggish river where sediment settles, blood components are more prone to clumping in veins, raising the risk of clot formation. For instance, many air travelers report swollen, heavy legs after a 5–6 hour flight—a telltale sign of impaired lower limb venous drainage.
Sitting for long hours playing cards: During holidays, gathering with loved ones for card games is a common pastime. Yet once absorbed in the game, people often sit motionless for hours, leaving their lower limbs inactive. The thrill of gameplay may also distract from physical fatigue or discomfort, further extending this stillness and creating ideal conditions for lower extremity DVT to develop.

(2) Dehydration
When traveling, people often drink too little and sweat excessively—their attention is fixated on enjoying scenery or having fun, so they frequently forget to hydrate properly. Moreover, during outings, the body loses significant amounts of sweat due to exercise, hot weather, or other factors. Without enough fluid replacement, blood thickens and flows more sluggishly. This viscous blood is far more prone to clotting in veins—much like how glue clogs a pipe far more easily than clear water.

(3) Dietary Factors
Holidays are naturally tied to delicious food—no celebration feels complete without it. People often load up on high-calorie, high-fat, and high-cholesterol fare: think fried snacks, pastries, or rich, fatty meats. These foods raise blood lipid levels, thickening the blood and making it more prone to clotting.
Additionally, excessive alcohol intake can disrupt the function of vascular endothelial cells (the delicate lining of blood vessels) and damage the integrity of blood vessel walls. Both changes create a pro-clot environment—further fueling DVT risk.
II. Typical Symptoms of Lower Extremity Deep Vein Thrombosis
(1) Lower Limb Swelling
This is one of the most common symptoms of lower extremity deep vein thrombosis. After a blood clot forms, it obstructs the return of venous blood from the lower extremities, causing blood to pool in the legs and leading to noticeable swelling.
The severity of swelling can vary from person to person. In mild cases, there may be slight edema in the calf or ankle: pressing on the area with a finger leaves an indentation that takes time to subside. In severe cases, the entire lower limb may swell dramatically—resembling an “elephant leg”—with tight, shiny skin and even blisters forming.
(2) Pain
Pain caused by lower extremity deep vein thrombosis (DVT) is typically a constant dull ache that worsens when standing or walking. This occurs because both activities increase resistance to venous return in the lower extremities and intensify irritation of the blood vessel walls by the clot.
The pain is mostly concentrated in areas with dense venous networks—such as the back of the calf or inner thigh. Some patients may also experience soreness in the lower limb muscles, similar to the ache after intense exercise, but it tends to be more severe and persistent, with no signs of relief.

(3) Elevated Skin Temperature
Due to obstruction of venous return in the lower extremities, impaired local blood circulation, and accumulation of metabolic waste, the affected lower limb develops elevated skin temperature. Upon touching the skin of the affected leg, it feels significantly warmer than the healthy (unaffected) side, and the skin may take on a slightly reddish hue. These changes in skin temperature and color are among the key physical signs of lower extremity deep vein thrombosis (DVT).

III. Risks of Lower Extremity Deep Vein Thrombosis
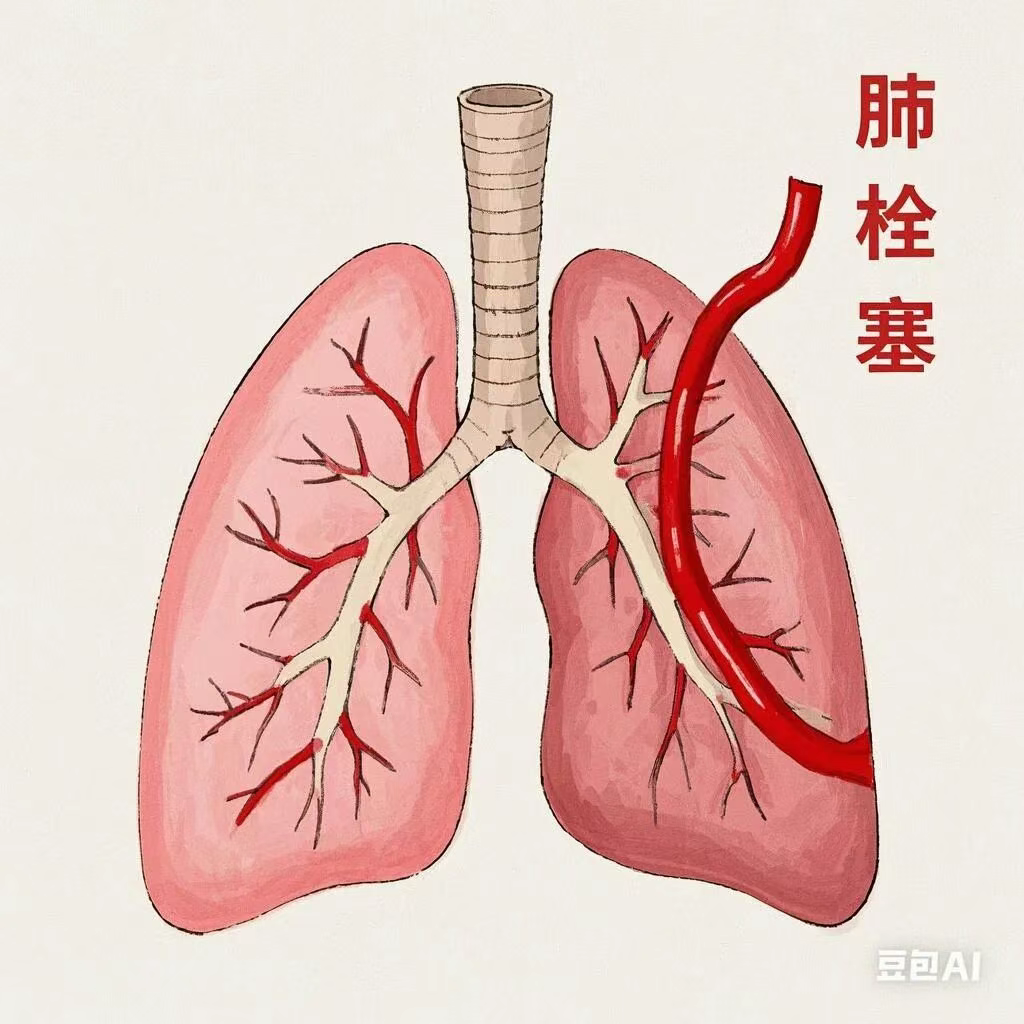
(1) Pulmonary Embolism (PE)
This is the most severe complication of lower extremity deep vein thrombosis (DVT) and one of the leading causes of death in affected patients.
When a clot partially or completely dislodges, it is carried by the bloodstream through the inferior vena cava (IVC), right atrium, and right ventricle, eventually reaching the pulmonary artery. There, it blocks the pulmonary artery and its branches—triggering pulmonary embolism (PE).
Pulmonary embolism can cause sudden onset of life-threatening symptoms, including dyspnea (shortness of breath), chest pain, hemoptysis (coughing up blood), and syncope (fainting). In severe cases, it can be fatal within minutes to hours.
Statistics show that ~50% of patients with untreated DVT will develop PE, and 10%–20% of those with PE will die from it.
(2) Chronic Lower Extremity Venous Insufficiency (CVI)
Even after treatment for lower extremity deep vein thrombosis (DVT), some patients may still develop chronic lower extremity venous insufficiency (CVI). This happens because the clot damages the structure and function of the venous wall and valves, leaving a lasting impairment in venous blood return.
Patients with CVI often experience long-term lower limb swelling, pain, skin hyperpigmentation (darkening), and ulcers—symptoms that severely diminish their quality of life. Over time, chronic venous insufficiency also causes skin nutritional deficits, making the skin thin, hardened, and prone to damage. Once the skin breaks down, wounds heal poorly and frequently progress to chronic ulcers, inflicting significant pain and distress on patients.
IV. What Should a Patient Do If They Have Lower Extremity Deep Vein Thrombosis (DVT)?
(1) Seek Medical Help Immediately
If you suspect you have lower extremity DVT, go to the hospital or see a doctor right away. To confirm the diagnosis, physicians usually:
•Take a detailed medical history,
•Perform a physical exam,
•Order tests like lower extremity vascular ultrasound or venography (an imaging test using contrast dye to visualize veins).
Early diagnosis and treatment are criticalto improving your prognosis. Never delay care—even if symptoms feel mild or you hope they’ll go away on their own.

(2) Drug Therapy
Anticoagulant Therapy: This is the cornerstone of DVT treatment. Anticoagulants—such as heparin, warfarin, and novel oral anticoagulants (NOACs)—work by inhibiting blood clotting, preventing the existing clot from expanding, and promoting gradual clot dissolution.
It is critical to take medications exactly as prescribed, regularly monitor coagulation parameters (e.g., INR for warfarin), and adjust doses based on test results to ensure both efficacy and safety. During anticoagulation, patients may experience bleeding tendencies (e.g., nosebleeds, gum bleeding, or skin bruising). Promptly inform your doctor if these occur—they may need to adjust therapy or address underlying issues.
Thrombolytic Therapy: For select patients in the acute phase (within 14 days of onset) with a high thrombus burden(large or extensive clots), doctors may consider thrombolysis. Thrombolytic drugs directly dissolve clots, restoring patency to blocked veins. However, this treatment carries a higher risk of bleeding, so it is only used when strict indications are met and under close medical supervision.
(3) Surgical Treatment
For the small subset of patients with severe DVT or poor response to drug therapy, surgery may be necessary. Common surgical approaches include:
•Thrombectomy: A procedure where the clot is surgically removed from the vein to immediately restore blood flow.
•Catheter-Directed Thrombolysis (CDT): A minimally invasive technique where a thin catheter is inserted into the clot site, delivering thrombolytic drugs directly to the clot. This enhances clot breakdown and reduces systemic bleeding risk compared to traditional thrombolysis.
Surgery can rapidly relieve symptoms, but it also carries risks (e.g., bleeding, infection). Doctors will perform a comprehensive evaluation of the patient’s overall health, clot severity, and treatment goals before recommending surgery.
V. How to Prevent Lower Extremity Deep Vein Thrombosis (DVT) During Holidays
(1) Avoid Prolonged Immobility
When traveling: Whether by car or plane, get up and move around every so often—walk a few steps down the airplane aisle, or stretch your legs when stopping at a highway rest area. Even if you can’t stand, do simple leg exercises in your seat: flex and extend your ankles, rotate your feet, or contract your calf muscles. These movements use muscle action to promote venous blood return from the lower limbs. Aim for a 5–10 minute activity break every 1–2 hours of sitting.
When playing cards or relaxing: Avoid sitting continuously at the table—take regular breaks (about once an hour) to stand up, walk around, and stretch your body. Use these pauses to move your lower limbs and boost circulation. You can also try gentle lower limb massages: start from your ankles and stroke upwards along your calves and thighs. This helps relax muscles and improve blood flow back to the heart.

(2) Stay Well-Hydrated
When traveling: Carry a water bottle and sip fluids regularly—don’t wait until you’re thirsty. By the time thirst hits, your body is already mildly dehydrated. Aim for 1,500–2,000 mL of fluids daily, prioritizing plain water or light tea. In hot weather or after heavy sweating, bump up your intake. If a packed itinerary makes on-the-go drinking tricky, prep high-water-content snacks like watermelon, cucumber, or cherry tomatoes beforehand—they hydrate andsneak in extra nutrients.
In daily holiday life: Build a habit of consistent hydration—even if you’re not traveling, don’t overlook fluids. This matters most when you’re sitting for hours (e.g., binge-watching shows, gaming): drink more to maintain your body’s fluid balance, thin your blood, and reduce viscosity (thickness).

(3) Healthy Diet
Control portion sizes and food choices: During holidays, watch your portions and avoid overeating. Cut back on high-calorie, high-fat, and high-cholesterol foods—like fried snacks, organ meats, and creamy pastries. Instead, boost your fiber intake with more fresh vegetables, fruits, and whole grains. These foods are rich in fiber, which helps improve gut motility, lower cholesterol, and reduce blood viscosity. Aim for ~500 grams of vegetables and 200–350 grams of fruit daily, for example.
Limit alcohol: Excessive drinking harms blood vessel health—so moderation matters during holidays. Men should keep alcohol intake to ≤25 grams of pure alcohol per day, and women to ≤15 grams. If you have cardiovascular disease or other chronic conditions, it’s best to avoid alcohol completely.

(4) Wear Appropriate Clothing
When traveling during holidays, opt for loose-fitting, comfortable clothes and shoes. Avoid tight-fitting pants, socks, or high heels—these can restrict lower limb movement, impair blood circulation, and raise your risk of DVT. This is especially crucial during long trips by car, plane, or train: loose clothing allows free movement of your legs and ensures smooth blood flow.
Conclusion
In short, while holidays are meant for relaxation, we must never overlook our health. By understanding the causes of DVT and taking proactive steps—like avoiding prolonged sitting, staying hydrated, and eating a balanced diet—we can enjoy the festive fun andeffectively prevent DVT, ensuring a healthy, happy holiday. If symptoms of DVT do occur, seek medical attention immediately, cooperate fully with treatment, and minimize the impact of the condition.
Preliminary Review: Zhang Jie
Final Review: Ma Shuqian
