World Alzheimer's Month | Early Prevention and Treatment, Safeguarding Cognition
World Alzheimer's Month | Early Prevention and Treatment, Safeguarding Cognition

Every September is World Alzheimer's Awareness Month. September 21, 2025, marks the 32nd "World Alzheimer's Day". This year's theme is "Early Prevention and Treatment, Safeguarding Cognition". It aims to guide the whole society to participate jointly, enhance public scientific understanding of dementia in old age, strengthen awareness of early detection, diagnosis, and intervention, and create a social atmosphere of caring for elderly people with dementia. Like an "eraser in the mind," it gradually erases patients' memories, cognition, and life skills, causing immense suffering not only to the patients themselves but also placing a heavy burden on families and society.
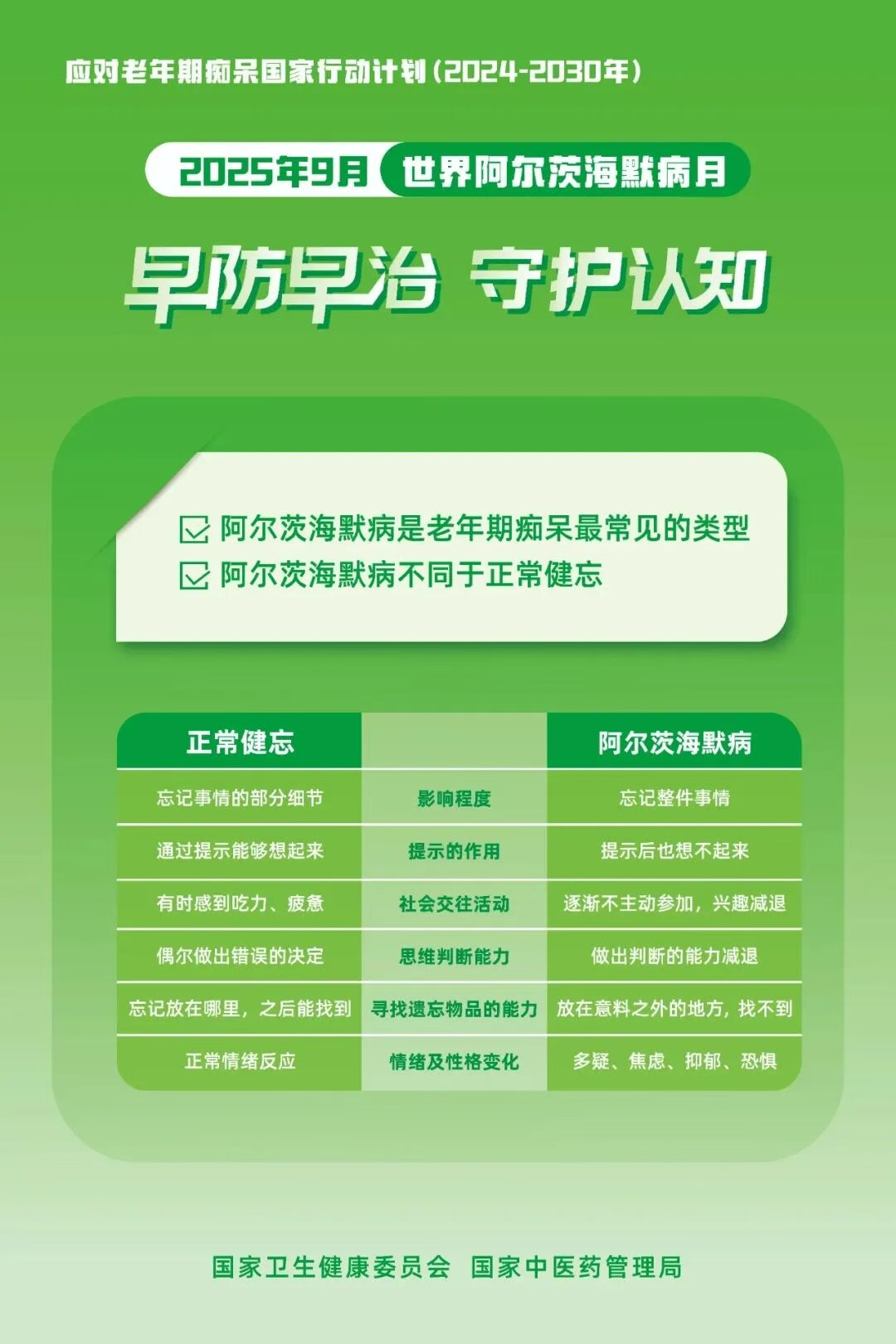
Alzheimer's Disease
Alzheimer's Disease (AD), also known as senile dementia, is a chronic, progressive degenerative disease of the central nervous system. Its main characteristics are the gradual decline of memory, cognitive function, and behavioral abilities, severely affecting patients' daily lives and work. According to World Health Organization data, over 46 million people worldwide suffer from Alzheimer's disease, with a higher incidence particularly among those over 65, placing a heavy burden on patients and their families. Relevant data shows that the prevalence of Alzheimer's disease among people aged 60 and above in China is approximately 3.9%, and the risk of developing the disease increases with age. Worryingly, due to insufficient public awareness of the disease, most patients are diagnosed in the middle or late stages, missing the optimal window for intervention. In fact, Alzheimer's disease does not "suddenly appear"; it releases "warning signs" years before onset. Scientific early identification and standardized diagnosis and treatment are key to managing Alzheimer's disease.

Clinical Manifestations of Alzheimer's Disease
Alzheimer's disease does not strike suddenly. Instead, as the disease progresses, patients experience functional decline in multiple aspects. These symptoms gradually worsen, seriously impacting the patient's life, as reflected in the following levels:
- Emotional and Memory Level
The most prominent feature is emotional apathy. Even facing major life events like parting or bereavement, patients may show little emotional fluctuation, which is a typical psychiatric manifestation of the disease. Simultaneously, memory loss is very pronounced. Patients are often forgetful, forgetting appointments made just days before, or even events that happened minutes ago. This severe forgetfulness leads them to repeatedly ask the same questions and often misplace items after handling them.
2.Cognitive and Behavioral Level
As the disease develops, gradual loss of brain neurons and dysfunction in neural networks affect cognitive function. Thinking becomes sluggish, understanding abstract concepts becomes difficult, and inattention and confusion occur frequently. Furthermore, neuronal death interferes with normal brain signaling, directly affecting emotion regulation, social behavior, and decision-making, leading to significant changes in personality and behavior. Patients may become irritable, depressed, or withdrawn, gradually losing interest in social activities.
3.Sense of Direction and Language
Function LevelSignificant abnormalities are also evident in sense of direction and language function. When going out, patients easily get lost or take long detours, as their ability to discern direction is greatly reduced. When language function is affected, patients struggle to correctly receive and express information, often confusing or misusing words or numbers during communication.
4. Ability to Live Independently Level
In the later stages of the disease, the ability to live independently gradually declines. Basic daily activities like dressing and bathing require assistance, and the ability to handle tasks such as shopping, cooking, and cleaning is significantly reduced. In severe cases, patients may even need help with eating.

Common Risk Factors for Alzheimer's Disease
Genetic Factors
Genetics is an important risk factor for Alzheimer's disease. If there is a family history of Alzheimer's, the disease may be passed on to the next generation. Once the disease is triggered, it significantly impacts the patient's normal life, disrupting their routine and causing numerous difficulties for the patient and their family.
Unhealthy Lifestyle Habits
Long-term unhealthy lifestyle habits increase the risk of developing Alzheimer's disease. For example, long-term heavy smoking damages multiple organs, including the brain, affecting its normal function; frequent excessive alcohol consumption harms the nervous system, disrupting normal neuronal activity; staying up late disrupts the body's biological clock, affecting normal metabolism and repair, thereby adversely impacting brain health; lack of exercise leads to decreased physical function and poor blood circulation, preventing the brain from receiving adequate nutrients and oxygen. These unhealthy habits acting together may induce Alzheimer's disease.
Age Factor
Increasing age is a significant and unavoidable risk factor for Alzheimer's disease. As age increases, the function of various organs gradually declines, and brain function is no exception. Brain nerve cells gradually decrease, the secretion and transmission of neurotransmitters become abnormal, and functions like cognition and memory gradually decline, significantly increasing the probability of elderly people developing Alzheimer's disease.
Recommendations for Diagnosis and Treatment of Alzheimer's Disease
For the diagnosis and treatment of Alzheimer's disease, it is recommended to prioritize the Neurology or Geriatrics departments of tertiary hospitals. Doctors will comprehensively assess the condition through "scale assessments + auxiliary examinations". Common examination items include:
- Cognitive Function Scales: Using scales like the "MMSE (Mini-Mental State Examination)" and "MoCA (Montreal Cognitive Assessment)" to test memory, attention, and language ability, providing a preliminary judgment of cognitive impairment severity.
- Blood Tests: Ruling out conditions like thyroid dysfunction, Vitamin B12 deficiency, and liver/kidney dysfunction that can cause "pseudo-dementia".
- Imaging Examinations: Head CT or MRI scans to observe if there is brain atrophy and exclude other brain pathologies like cerebral infarction or brain tumors.
- Biomarker Testing: Detecting Alzheimer's-related proteins in the brain (such as beta-amyloid and tau proteins) to improve diagnostic accuracy.
How to Prevent and Intervene Early in Alzheimer's Disease
- Adopt a Healthy Lifestyle: Cultivate exercise habits and hobbies, eat healthily, quit smoking and limit alcohol, engage in continuous learning, use the brain frequently, participate in social activities, maintain an optimistic outlook, and avoid social isolation.
- Reduce Risk Factors: Individuals with mid-life obesity, hypertension, diabetes, stroke, depression, hearing loss, or a family history of dementia should pay extra attention to controlling weight, correcting hearing loss, and maintaining healthy blood pressure, cholesterol, and blood sugar levels.
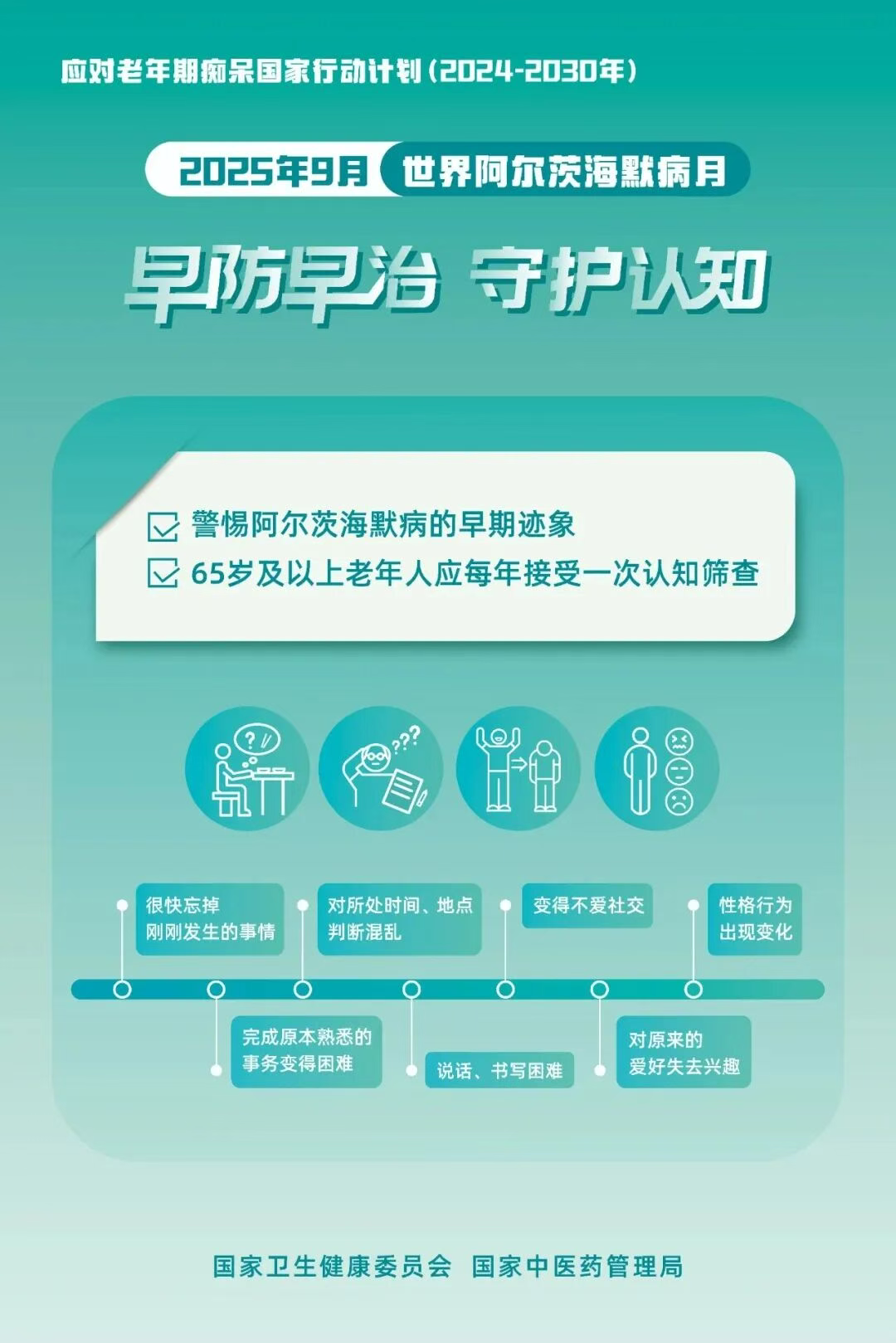
- Know the Early Signs of Alzheimer's Disease: These include: quickly forgetting recently learned information; difficulty completing familiar tasks; confusion about time or place; trouble with vocabulary, speaking, or writing; withdrawal from social activities and loss of interest in hobbies; changes in personality or behavior.
- Seek Medical Attention Promptly: If early signs of Alzheimer's appear in an elderly person, family members should promptly accompany them to seek medical care at the geriatrics department, neurology department, psychiatry/psychology department, memory clinic of a general hospital, or a specialized mental health hospital.
- Pursue Active Treatment: Drug and non-drug treatments can help improve cognitive function, reduce complications, enhance quality of life, and lessen the burden on caregivers. Under professional guidance, non-drug therapies such as sensory stimulation, physical and cognitive exercise, music therapy, and environmental therapy can be implemented.
- Provide Good Family Care: Family members should learn communication skills, caregiving techniques, and methods for managing negative emotions. In daily life, assist without taking over completely to help maintain the patient's existing abilities. Provide a safe living environment, consider using anti-wandering devices, prevent injuries, and prevent the patient from getting lost.
- Respect the Patient's Dignity and Basic Rights: Focus on emotional support, avoid hurting their self-esteem, communicate with a kind attitude, and do not easily dismiss their requests. Respect the patient and, under the premise of safety, give them as much autonomy and freedom as possible.
- Support Caregivers: Caregivers of patients experience significant physical and mental pressure. Provide professional care training and support services to caregivers to protect their physical and mental health.
- Create a Supportive Social Environment: Strengthen social awareness campaigns, reduce discrimination against patients, care for patients and their families, and build a dementia-friendly social environment.
"Early prevention and treatment, multi-pronged approach" is the core principle in combating Alzheimer's disease. Although there is currently no cure, through scientific drug treatment, reasonable nutritional support, and active lifestyle interventions, we have the full capacity to effectively slow disease progression and improve patients' quality of life.
