Radiotherapy Diet Guide: Alleviating Side Effects and Recharging the Body
I. Potential Physical Reactions After Radiotherapy
Radiotherapy is a crucial method for treating tumors, using precise radiation to kill cancer cells, but it may cause some side effects, broadly categorized into two types:
1.Localized Reactions (Symptoms at the Radiation Site)
• Skin and Mucosal Damage: Radiation sites may exhibit redness, dryness, peeling, and in severe cases, blisters or ulcers. Post-healing, hyperpigmentation may occur.

Organ-Specific Effects:
• Digestive Tract (e.g., abdominal radiotherapy): Nausea, vomiting, diarrhea, or difficulty swallowing.
• Chest (e.g., lung cancer radiotherapy): Cough, chest tightness, or breathing difficulties (radiation pneumonitis).
• Head and Neck (e.g., nasopharyngeal cancer radiotherapy): Dry mouth, oral infections.
• Pelvis (e.g., colorectal cancer radiotherapy): Diarrhea, frequent urination, painful urination.
2.Systemic ReactionsDuring radiotherapy, the body may experience systemic symptoms due to radiation stimulation and tumor cell necrosis:
• Fatigue: Persistent exhaustion that persists despite rest, linked to increased energy expenditure.
• Decreased Immunity: Reduced white blood cells and platelets, leading to susceptibility to infections, bleeding, or pallor.
• Emotional Impact: Anxiety or depression, potentially affecting appetite and quality of life.
Clinically, doctors develop personalized plans based on the patient’s condition. Supportive therapies (e.g., skin care, nutritional support, leukocyte-boosting treatments) help mitigate side effects. Most patients gradually recover post-treatment. Close collaboration with medical staff and timely reporting of discomfort are essential for optimal outcomes and quality of life.
How to Supplement Nutrition for Advanced Cancer Patients

Advanced cancer patients often experience malnutrition due to disease-related metabolic demands and treatment side effects (e.g., reduced appetite, impaired digestion and absorption). Proper nutrition is crucial for maintaining physical strength, improving quality of life, and supporting treatment tolerance. Scientific dietary management and balanced nutrition are essential. Patients should follow the principle of "rational intake with evidence-based restrictions" in daily meals.
I. Principles of Nutritional Supplementation
1.Focus on High-Calorie, High-Protein Foods:Prioritize easily digestible, high-protein foods such as eggs, milk, lean meat (pork/beef/lamb), fish (e.g., crucian carp, perch), soy products (tofu, soy milk), and protein powder (used under medical guidance). These aid tissue repair and enhance immunity.

2.Balanced and Diverse Diet:Ensure intake of grains (e.g., millet, rice, oats), fresh vegetables (leafy greens, mushrooms), and fruits (e.g., apples, bananas, kiwifruit) to provide vitamins, minerals, and dietary fiber, promoting intestinal motility.
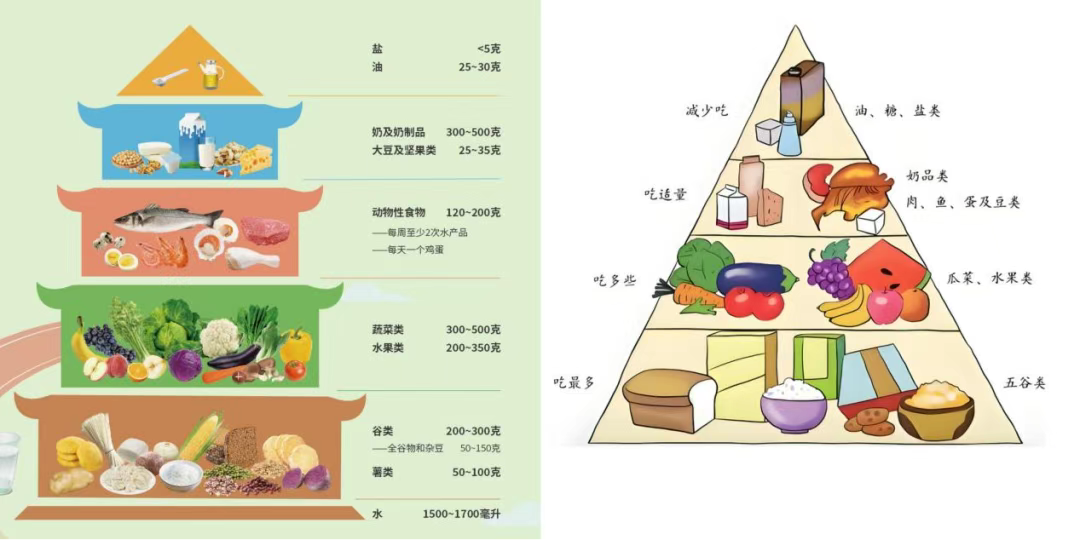
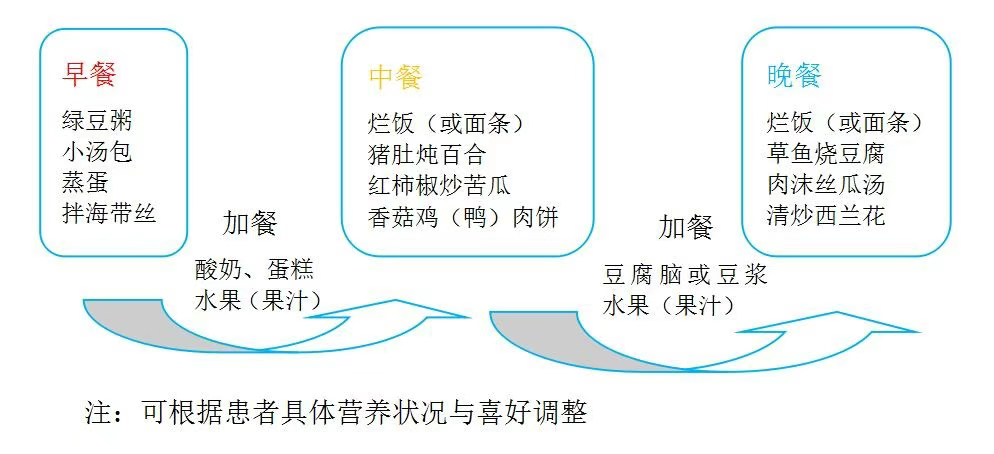
3.Small, Frequent Meals with Soft, Easily Digestible Foods:For poor appetite, split 3 daily meals into 5–6 smaller ones. Choose soft, liquid, or semi-liquid foods (e.g., porridge, noodle soup, steamed egg custard, minced meat with vegetable puree) to reduce gastrointestinal burden.
II. Targeted Adjustments
1.Weak digestive function: Avoid greasy, spicy, or raw/cold foods. Cook foods until soft and tender; if necessary, use enteral nutrition preparations (e.g., nutritional liquids) for supplementation.
2.Difficulty swallowing: Choose paste-like foods such as thick porridge, lotus root starch paste, or sesame paste. Alternatively, blend foods into a puree to avoid choking.

3.Altered taste: Adjust flavors appropriately (e.g., use natural seasonings sparingly) but avoid excessive saltiness or sweetness. Ensure food temperature is suitable (avoid scalding).
III. Key Considerations
1.If experiencing severe eating difficulties or malnutrition, seek medical or dietitian guidance for supplementation via nasogastric tube feeding or intravenous nutrition. Avoid forcing food intake.
2.Refrain from unnecessary dietary restrictions ("avoidance") unless explicitly advised by a doctor (e.g., specific treatments requiring food limitations). Over-restriction may lead to nutrient deficiencies.
3.Prioritize patient preferences to enhance willingness to eat. Family members may assist in preparing diverse and appealing meals.
4.Avoid foods that may accelerate disease progression or carry carcinogenic risks. Examples include processed meats—classified as Group 1 carcinogens—such as sausages, ham, and smoked bacon. These contain nitrites and polycyclic aromatic hydrocarbons, which are carcinogenic and may worsen tumor conditions. Minimize or eliminate consumption.

IV. Key Reminders
Nutritional supplementation requires individualization. Patients are advised to communicate with their attending physician or clinical dietitian to develop a personalized plan based on their specific condition, weight changes, digestive function, etc. Avoid blind self-supplementation.
For inquiries, please contact us:
The Radiotherapy Department I of Wuwei Cancer Hospital specializes in carbon-ion and photon radiotherapy for abdominal/pelvic malignancies (e.g., liver cancer, cholangiocarcinoma, pancreatic cancer, colorectal cancer, renal cancer, prostate cancer). We also provide comprehensive treatments including chemotherapy, targeted therapy, immunotherapy, and cellular immunotherapy. Currently, our department is conducting a clinical study on carbon-ion radiotherapy for early-to-mid-stage hepatocellular carcinoma (HCC). Eligible participants may receive carbon-ion therapy free of charge.
Preliminary Review: Ma Shuqian
Final Review: Zhang Lihong
