Male patient, malignant tumor at the base of the tongue
Unresectable Tongue Base Cancer Treated with Heavy Ion Therapy
Tongue base cancer predominantly affects males, with a male-to-female ratio of approximately 2–5:1. However, the incidence in females has been rising in recent years, which may be correlated with the increasing number of female smokers. The disease typically occurs in older age groups, with the highest prevalence among individuals aged 50–70. Over the past two decades, the development of tongue base cancer has been closely linked to HPV infection.
For stage I and II patients without regional lymph node metastasis, both surgery and radiotherapy can achieve curative outcomes. However, radiotherapy preserves masticatory and swallowing functions and is therefore preferred. For stage III and IV patients, a comprehensive treatment approach combining surgery and radiotherapy is recommended. Chemotherapy remains an adjuvant treatment, used preoperatively, postoperatively, or in conjunction with radiotherapy, or as palliative treatment for advanced cases. Carbon ion radiotherapy (CRIT) is an emerging radiotherapy modality in the 21st century. Compared to traditional X-ray radiotherapy, carbon ion therapy offers significant therapeutic advantages and is internationally recognized as one of the most effective cancer treatment methods. It boasts high precision, minimal side effects, reduced damage to normal tissues, high cure rates, and shorter treatment cycles. Due to its high energy and strong tumor-killing capability, carbon ions can precisely destroy tumor cells while causing less damage to surrounding healthy tissues. This makes carbon ion therapy particularly advantageous for treating specific types of tumors, especially deep-seated tumors and those adjacent to critical organs (such as the optic nerve, brainstem, and lens), or for preserving organ function. Below is a case of tongue base cancer treated with heavy ion therapy.
Medical History
The patient was admitted due to intermittent fatigue and pharyngeal pain lasting one year. One year prior to admission, the patient developed pharyngeal pain and fatigue without headaches or dizziness. In February 2024, electronic nasopharyngoscopy revealed chronic hyperemia of the pharyngeal mucosa with scattered lymphoid follicle hyperplasia and multiple pale pink neoplastic growths on the left tongue base. The diagnostic suggestion was chronic pharyngitis and possible tongue base papilloma. Subsequent repeated pharyngoscopies failed to confirm the diagnosis. On December 4, 2024, electronic laryngoscopy showed lymphoid follicle hyperplasia at the tongue base. The lingual surface of the epiglottis was adherent to the left side of the tongue base, preventing full exposure, and a pale pink, rough-surfaced neoplasm was observed on the left lingual surface of the epiglottis. The diagnostic suggestion was epiglottic tumor and chronic pharyngitis. A neck CT indicated a left tongue base mass measuring approximately 28×27 mm, suggestive of malignancy, with multiple enlarged left cervical lymph nodes, the largest measuring about 20×26 mm. On December 15, 2024, a neck MRI revealed an abnormal signal in the left tongue body, measuring approximately 38×33×39 mm, suggestive of malignant tumor, with multiple enlarged lymph nodes in the left carotid space, the largest with a short axis of about 14.7 mm, indicative of metastasis. On December 19, 2024, a biopsy of the tongue base mass showed atypical epithelial nests within proliferative fibrous tissue, consistent with infiltrating squamous cell carcinoma.
Admission Diagnosis: Malignant tumor of the tongue base; squamous cell carcinoma; cT3N2bM0, stage IVA; KPS score: 80.
Treatment Course
- Jaw and neck MRI: A mass with enhancement was observed in the tongue base and left tongue body, with the largest cross-sectional size of approximately 3.8×2.4 cm, suggestive of a neoplastic lesion. The epiglottis and left submandibular gland were involved. Several enlarged lymph nodes were noted in the left submandibular and cervical root areas, suggestive of metastasis, with the largest measuring approximately 1.5×1.8 cm. Tubular shadows were observed in the bilateral submandibular glands, suggestive of ductal dilation. Multiple small lymph nodes were noted in the bilateral submandibular, cervical vascular spaces, and bilateral cervical root areas.
- Carbon ion irradiation was employed with the following prescription doses: GTV: 68 Gy (RBE)/17 fractions, 4 Gy (RBE)/fraction; PTV1: 60 Gy/15 fractions, 4 Gy/fraction; PTV2: 56 Gy/14 fractions, 4 Gy (RBE)/fraction.
- During radiotherapy, the patient developed grade 2 radiation-induced oral mucositis (RTOG) and grade 2 acute radiation dermatitis (RTOG), both of which resolved within two weeks of treatment.
Efficacy Evaluation
Pre-treatment
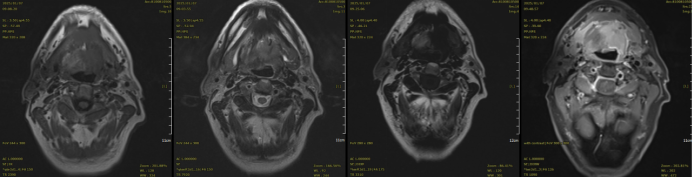
Pre-treatment MRI: A mass was observed in the tongue base and left tongue body, with the largest cross-sectional size of approximately 3.8×2.4 cm. The tongue base and left tongue body showed enhancement, suggestive of a neoplastic lesion. The epiglottis and left submandibular gland were involved. Several enlarged lymph nodes were noted in the left submandibular and cervical root areas, suggestive of metastasis.
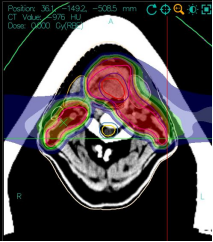
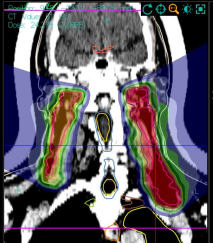
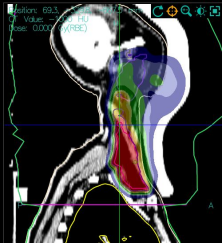
Carbon ion therapy dose cloud chart.
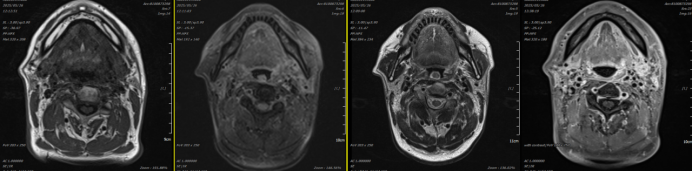
Post-treatment MRI (3 months): A small patchy long T1 and slightly long T2 signal was observed in the tongue base, with the largest cross-sectional size of approximately 1.0×1.5 cm. DWI showed no restricted diffusion, and enhancement scanning revealed heterogeneous enhancement. Multiple lymph nodes were observed in the bilateral submandibular and cervical vascular spaces and bilateral cervical root areas, with the largest located in the left cervical root, measuring approximately 0.7×1.0 cm.
Efficacy evaluation: The tumor size was significantly reduced compared to pre-treatment, with a clinical assessment of partial response (PR).
Discussion
Oral cancers, including tongue base cancer, are relatively hypoxic and less sensitive to conventional treatments. The relative biological effectiveness (RBE) of heavy ions is 2–3 times that of traditional radiotherapy, making it particularly effective against radiotherapy-resistant hypoxic cells and recurrent tumors. Additionally, the incidence of severe oral mucositis is reduced by 40%, with improved patient tolerance and significantly enhanced quality of life. In the treatment of oral cancers, carbon ions markedly reduce radiation doses to surrounding normal tissues (e.g., salivary glands, jawbone, spinal cord). Carbon ion therapy can reduce spinal cord exposure to less than 1/6 of that from traditional photon therapy. Clinical data show that local control rates for oral cancer patients treated with carbon ions increase to 70%–80%, with reduced recurrence risk. For recurrent or refractory oral cancers, the 5-year survival rate with carbon ion therapy can reach 50%–60%, compared to only 30%–40% with traditional photon therapy.
