Female, 47 years old, recurrent high-grade glioma
Adult patient with recurrent high-grade glioma had a near total tumour elimination after chemotherapy
Description of medical history
The patient, female, 47 years old, presented in September 2023 with sudden onset of speech inability and numbness of the right limb. Cranial magnetic resonance imaging (MRI) showed left frontotemporal lobe and insula lesion, with a size range of about 5.6×6.0×4.8 cm, moderate peritumoural oedema, and the combination of MRS and DTI suggested high-grade glioma, with a high likelihood of glioblastoma. Cerebral hemispheric resection was carried out under general anaesthesia on 22 September 2023, and the results of the postoperative examination suggested (intracranial) oligodendroglioma, with increased cell density and heterogeneity in some areas, and mesenchymal oligodendroglioma, WHO grade 3, which was found in the left side of the brain. increased heterogeneity, mesenchymal oligodendroglioma, WHO grade 3. Immunohistochemical staining: tumour cells showed GFAP(-), Vimentin(+), S-100(+), Olig-2(+), EMA(-), Syn(+), Neun(-), CK(-), p53(wild type), ATRX(+), INI-1(+), H3K27M(-), IDH-1(+), Ki-67. Number of positive cells in the hyperplastic active zone 20%. Postoperative IMRT was initiated on 26 October 2023 at the prescribed doses of PTV1 D95%: 46 Gy/23 fx and PTV2 D95%: 14 Gy/7 fx. Simultaneous temozolomide chemotherapy was administered. After chemotherapy, 6 cycles of ‘bevacizumab injection + temozolomide’ were administered, during which the cranial MRI did not show any obvious signs of recurrence or metastasis.
Treatment
In December 2024, the patient developed numbness and weakness of the right hand and pain in the right lower limb appeared, and on 31 December 2024, the cranial nuclear magnetic resonance examination suggested that: the left frontotemporal insula surgery area residual cavity old blood accumulation part of the peripheral gliosis and edema changes, the supratentorial ventricles are widened (the left lateral ventricle is the prominent), the periphery of the lateral ventricles bilaterally, the knee of the corpus callosum has multiple enhancing nodular lesions and the surrounding large-scale edema, which is newer than the previous, and the tumour was considered to be mostly Recurrence. 4 cycles of chemotherapy with bevacizumab injection + temozolomide + etoposide. cranial MRI on 1 April 2025: postoperative glioma, post radiotherapy review, left frontotemporal insula operative area residual cavity with effusion, blood accumulation, and part of the peripheral gliosis with oedema, episcleral ventricle widening (left lateral ventricle is notable), compared with the previous (2024-12-31), the scope of oedema is narrowed; bilateral lateral ventricles around the knee of the corpus callosum, Multiple abnormal signal shadows with oedema in the knees of the corpus callosum, the degree of enhancement of the lesion is significantly reduced compared with the previous lesion, and some enhancement reveals poor clarity, and the peripheral oedema is reduced.
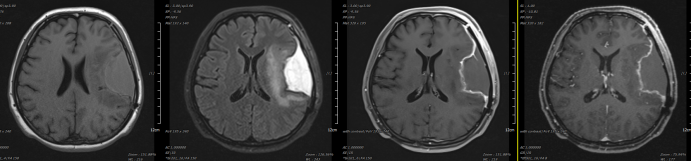
Figure 1: Cranial MRI after surgery on 2023-10-24: The patient is a postoperative glioma: localised absence of the left frontoparietal temporal bone, swelling of the left maxillofacial and temporal soft tissues with intramural fluid signals within them, cystic foci in the operative area, mostly considered as postoperative cystic cavities (blood?), and a large area of edema in the left insula and left temporal lobe. With large edema in the medial part of the operative area, please take into account the clinic; abnormal signals in the left insula and the left temporal lobe, mostly consider postoperative residuals.
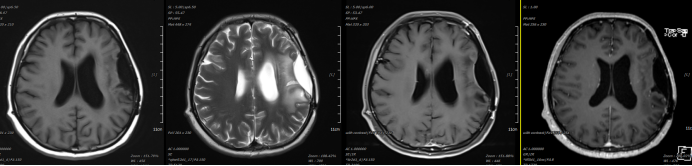
Figure 2: 2024-09-27 Review of cranial MRI 9 months after treatment: postoperative review of left frontotemporal lobe and insula glioma, gliosis and oedema changes around the residual cavity of the left frontotemporal-insular region of stale blood accumulation partially, and widening of the supratentorial ventricles. Abnormal signals in the left insula and left temporal lobe, roughly similar.
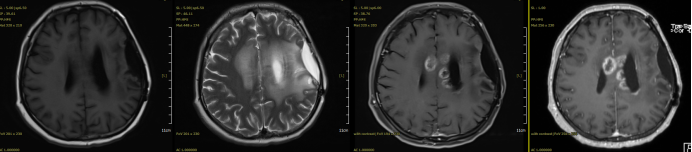
Figure 3: 2024-12-31 Review of cranial MRI 1 year after treatment: left frontotemporal lobe and insula glioma postoperative review, left frontotemporal insula operated area of residual cavity of old blood accumulation partially surrounded by gliosis and oedema changes, and widening of the curtain ventricle. Bilateral lateral ventricles around the knee of the corpus callosum multiple enhancing nodular shadows and surrounding large edema, more than the previous new out, more than the consideration of tumour recurrence.
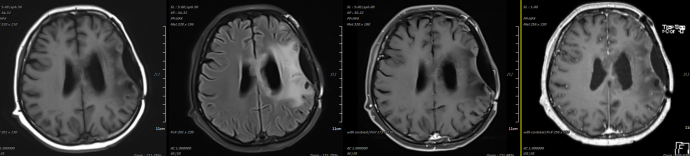
Figure 4: MRI after 4 cycles of targeted combination chemotherapy after recurrence on 2024-04-01: left frontotemporal insula operated area residual cavity with effusion, blood accumulation, and part of peripheral gliosis with oedema. Bilateral lateral ventricles around the knee of the corpus callosum, multiple abnormal signal shadow with edema, compared with the previous degree of enhancement of the degree of the lesion is significantly reduced, part of the enhancement of the display is unclear, the surrounding edema to reduce.
Expert Opinion
Oligodendrogliomas, rare primary brain tumours, are diffuse gliomas, and specimens of this tumour must be able to detect both isocitrate dehydrogenase (IDH) mutations and 1p/19q co-deletions. Depending on the histological features, they are classified as WHO-grade 2 or 3. Oligodendrogliomas, which are uncommon, account for approximately 5% of all neuroepithelial tumours of the central nervous system. It is usually found in adults between the ages of 25 and 45 years, and is occasionally detected in adolescents and adults over the age of 65 years. In contrast to other diffuse gliomas, oligodendrogliomas are highly sensitive to chemotherapy. The mechanism for the high sensitivity may be largely related to metabolically induced epigenetic changes, including: hypermethylated phenotype of CpG islands (CIMP) and promoter methylation of O6-methylguanine-DNA methyltransferase (MGMT). Although most patients are incurable and eventually leave, the natural history of oligodendrogliomas is long and oligodendrogliomas are more sensitive to both radiotherapy and chemotherapy than other IDH-mutant gliomas. For patients who cannot be treated with radiotherapy, sometimes only chemotherapy can be used. For example, patients with diffuse, multilobar involvement, or bilateral hemispheric oligodendrogliomas that would require extensive or whole-brain radiotherapy, or essentially whole-brain radiotherapy, may be treated with chemotherapy alone. Treatment of recurrent oligodendrogliomas and prognosis should be individualised according to previous treatment, location and resectability of the recurrent disease, and the time since the last radiotherapy. Despite the long, long survival time of oligodendrogliomas, almost all patients have a limited life expectancy due to tumour recurrence, eventual accelerated growth, and tumour resistance to available therapies. The average survival of, oligodendrogliomas in prospective trial results, is about 15 to 20 years. This case recurred 1 year after surgery, radiotherapy and chemotherapy, which is a poor survival. For poor survival, some of the more common clinical features include: older age, male, poor functional status, and/or baseline neurological deficits, non-epileptic manifestations, tumour location outside of the frontal and parietal lobes, and large tumour size (i.e., more than 4 to 5 cm). Limited data suggest that microvascular proliferation, necrosis, nuclear division number and Ki-67 labelling index remain prognostically significant as risk factors for shorter survival in IDH mutation with 1p/19q co-deletion type mesenchymal oligodendrogliomas. In addition, the presence of a pure CDNK2A/B deletion, which is a poor prognostic marker, is almost always present in grade 3 tumours.
