From Palliative to Curative ——Complete Remission of Maxillary Sinus and Liver Metastases
From Palliative to Curative: Complete Regression of Maxillary Sinus Carcinoma and Hepatic Metastases

Lu Jing
Chief Physician
Department of Radiotherapy, Lanzhou Branch (Lanzhou Heavy Ion Center)
Gansu Wuwei Cancer Hospital
——Radiologic Complete Response of Maxillary Sinus and Hepatic Lesions Achieved with Carbon-Ion Radiotherapy
In April 2023, Mr. Wang presented with when a progressively enlarging mass developed beneath his left orbital region, accompanied by left facial numbness, pain, and even difficulty opening his left eye. Upon referral from acquaintances, he sought evaluation at the Heavy Ion Hospital.
Maxillary sinus MRI revealed:
- A left maxillary sinus mass extending medially into the nasal cavity with ill-defined borders involving nasal turbinates and the ethmoid sinus
- Lateral extension obscuring demarcation from cheek musculature
- Superior invasion of the orbital floor involving left maxillary bone, alveolar bone, maxillary sinus walls, and medial orbital wall
- Lateral infiltration into left cheek tissue
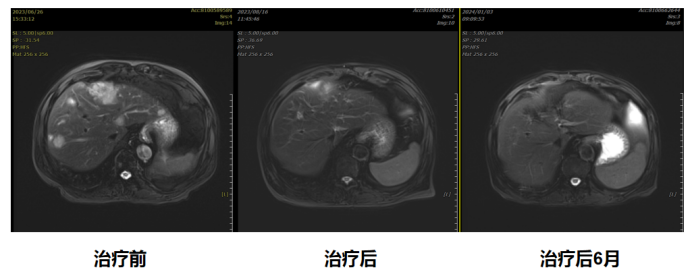
Abdominal MRI screening further demonstrated multiple suspicious nodules in hepatic segments SIV, SV, and SVIII, with the largest measuring 3.7 × 3.8 cm, highly suggestive of metastatic lesions. Subsequent pathological confirmation established the diagnosis of adenocarcinoma, a histologically radioresistant subtype.
Following multidisciplinary team (MDT) evaluation and detailed consultation regarding the unique advantages of heavy ion radiotherapy with Mr. Wang and his family, treatment commenced in May 2023. The therapeutic protocol comprised included 20 precisely fractionated heavy ion therapy sessions or maxillary sinus carcinoma and 12 ablative fractions for hepatic metastases.
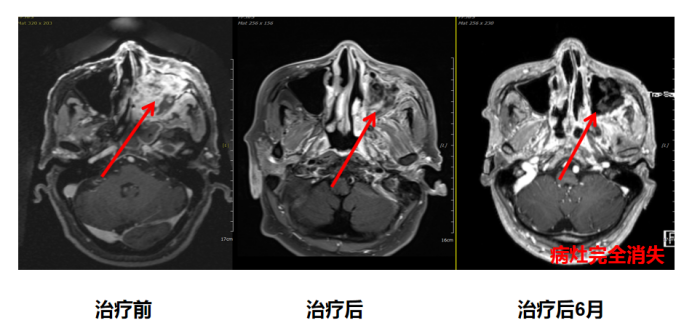
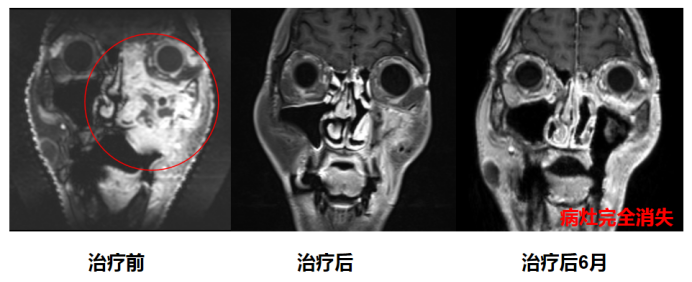
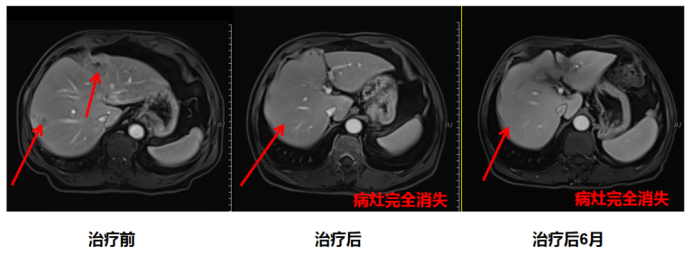
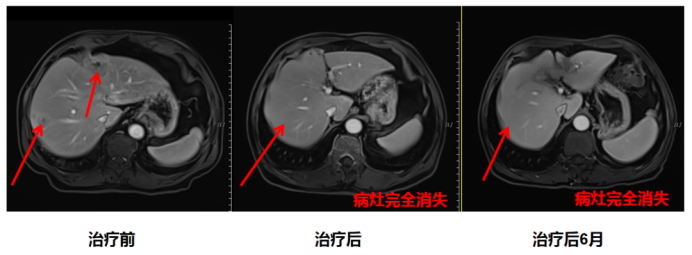
Notably, by the fifth treatment session, substantial regression of the infraorbital mass was observed. Post-treatment MRI demonstrated a 50% volumetric reduction in the maxillary sinus tumor and remarkably, complete resolution of hepatic metastatic foci. Mr. Wang subsequently continued structured systemic antitumor therapy to optimize clinical outcomes.
Following multidisciplinary team (MDT) consensus and comprehensive patient-family education regarding the dosimetric advantages of heavy ion therapy, Mr. Wang elected to proceed with this cutting-edge modality. In May 2023, his personalized treatment protocol was implemented, delivering 20 precisely targeted fractions to the maxillary sinus carcinoma and 12 ablative fractions to hepatic metastases using scanned carbon-ion beams.
Clinically significant response emerged remarkably early: by the fifth fraction, near-complete resolution of the infraorbital mass was documented. Post-treatment volumetric MRI analysis demonstrated a 50% reduction in gross tumor volume (GTV) of the primary lesion, with more striking radiologic complete response (CR) observed in hepatic metastases. Subsequently, Mr. Wang initiated adjuvant systemic therapy per NCCN-guided treatment algorithms to consolidate therapeutic gains.
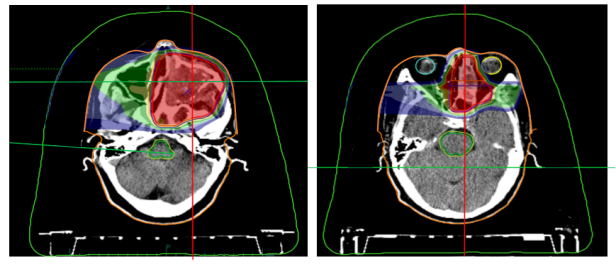
Beam direction and dose distribution of heavy ion radiotherapy target area for maxillary sinus cancer

Evaluation of Treatment Outcomes for Maxillary Sinus Cancer
Beam Angle Optimization and Bragg Peak-Dose Conformity in Carbon-Ion Radiotherapy Planning for Hepatic Metastases
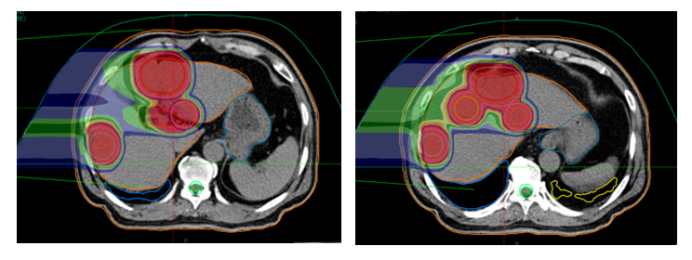

Evaluation of Treatment Outcomes for Hepatic Metastatic Carcinoma
Can Stage IV Cancer Patients with Distant Metastases Achieve Survival Benefit Through Local Radiotherapy? Carbon-ion radiotherapy (CIRT) leverages unique physical and biological properties to maximize tumor cell eradication. Its high linear energy transfer (LET) induces clustered DNA damage, with >70% of double-strand breaks (DSBs) exhibiting ≥2 lesion sites per chromatin domain, overwhelming cellular repair mechanisms. These radiobiological advantages translate to superior local control rates (LCRs), which may confer long-term survival benefits in oligometastatic disease. A landmark 2016 Lancet Oncology study compared metastasis-directed radiotherapy versus maintenance chemotherapy: the radiotherapy arm demonstrated median progression-free survival (PFS) of 11.9 months versus 3.9 months in the chemotherapy group. Irradiation of both primary and oligometastatic lesions significantly delays systemic progression, thereby extending overall survival (OS).
The oligometastatic paradigm, conceptualized by radiation oncologist Samuel Hellman, describes an intermediate state between localized and widely metastatic disease. Originally defined as ≤5 metastases in ≤3 organs, this state represents limited tumor burden resulting from vascular dissemination of micrometastases to specific organ niches. Timely local interventions during this "window of curability" can achieve durable disease control.
For this patient presenting with hepatic metastases, our carbon-ion-based multidisciplinary protocol achieved: effective tumor burden reduction through ablative CIRT doses (≥60 Gy [RBE] to hepatic lesions) prevention of locoregional complications including: dysphagia/airway obstruction from rapid skull base progression, cranial neuropathies from perineural invasion, hepatic failure/biliary obstruction from metastatic expansion, foundation for systemic synergy via planned integration with PD-1 immunotherapy, tyrosine kinase inhibitors, and metronomic chemotherapy, current surveillance confirms no evidence of disease progression at treated sites. We maintain vigilant molecular monitoring while implementing NCCN-guided maintenance therapy to sustain this asymptomatic remission state.
Professor Junjie Wang's Clinical Research Team
Lanzhou Heavy Ion Center

Wang Junjie
Chief Physician, Professor
Currently serves as Director of the Department of Radiation Oncology at Peking University Third Hospital, Doctoral Supervisor, Director of the Brachytherapy Center at Peking University Health Science Center, and Deputy Director of the Department of Radiation Oncology at Peking University.
Chairman of the 10th Committee of the Society of Radiation Oncology, Chinese Medical Association.
Inaugural Chairman of the Brachytherapy and Intelligent Radiotherapy Society of the Chinese Nuclear Society.
Vice Chairman of the Minimally Invasive Therapy Committee of the Chinese Anti-Cancer Association.
Chairman of the Radioactive Particle Ablation Technology Committee of the National Strategic Alliance for Technological Innovation in Tumor Minimally Invasive Therapy Industry.
Associate Editor-in-Chief of the Chinese Journal of Radiological Medicine and Protection.
Editorial Board Member of the American journal Brachytherapy.
Li Xiaojun
Chief Physician, Vice President
Currently serving as Assistant Dean of Gansu Province Wuwei Cancer Hospital and Vice President of Lanzhou Proton and Heavy Ion Hospital.
Gansu Province Longyuan Youth Talent, Gansu Province Health Industry Outstanding Youth Talent.
Heir of Traditional Chinese Medicine (TCM) at Gansu Provincial Health Commission.
Visited the RPTC Proton Center in Munich, Germany; studied at the Shanghai Proton and Heavy Ion Hospital, Beijing Cancer Hospital, Sichuan Cancer Hospital, and the Varian Training Center in the USA.
Specializes in radiation therapy for tumors of the central nervous system, head and neck, chest, abdominal and pelvic regions, and extremities.
Awarded the Second Prize of Gansu Provincial Science and Technology Progress and multiple science and technology progress awards in Wuwei.
Led and participated in over 10 provincial and municipal research projects, including major provincial science and technology special projects and key talent programs of the Provincial Party Committee Organization Department.
Published 7 SCI papers as the first/corresponding author and over 30 papers in domestic core journals; holds 10+ invention and utility model patents for radiation therapy.
Clinic Schedule: Monday to Friday, 5th Floor of the Inpatient Department, Lanzhou Campus.

