New Breakthrough in the Treatment of Odontogenic Ghost Cell Carcinoma - Heavy Ion Therapy
New Breakthrough in the Treatment of Odontogenic Ghost Cell Carcinoma - Heavy Ion Therapy
The patient is a 36-year-old male, with the chief complaint of recurrence of odontogenic ghost cell carcinoma in the left maxilla, more than 2 months after multiple surgeries.
**Present Illness:**
The patient underwent "maxillary cyst removal" on May 8, 2023, due to a left maxillary mass. Postoperative pathology reported "odontogenic calcifying epithelial tumor." In January 2024, the patient experienced pain in the left maxillary teeth, swelling in the left nasal and maxillary regions, and a biopsy of the left maxilla indicated: ① odontogenic calcifying epithelial tumor; ② malignancy could not be completely ruled out. On January 30, 2024, the patient underwent "exploration and resection of the left maxillary mass, partial maxillectomy, gingival flap surgery, local tissue flap transfer repair, and nerve dissection." Pathological diagnosis confirmed a malignant tumor of the left maxilla, consistent with odontogenic ghost cell carcinoma based on morphology and immunohistochemistry. Immunohistochemistry results: tumor cells were positive for CK5/6(+), p63(+), p40(+), CK19(+), p16(+), weakly positive for p53, and negative for S100, CR, BRAF V600E (VE1), and PTEN. PHH3 (>20/10HPF) and Ki-67 (approximately 60% in hotspot areas) were positive. Special staining results: Congo red (pre-oxidation) (-), Congo red (post-oxidation) (-).
In April 2024, the patient developed left facial pain and left eye tearing, with worsening pain. On April 25, 2024, the patient underwent "expanded exploration and resection of the left maxillary mass, partial maxillectomy, tooth extraction, nerve dissection, titanium plate implantation, fibular myocutaneous flap transfer repair, and vascular anastomosis." In June 2024, a mass reappeared on the left nasal dorsum, with left nasal dorsum swelling and mild tenderness on palpation. On July 29, 2024, the patient underwent "expanded resection of the left nasal mass, partial resection, forehead flap transfer repair, and local tissue flap transfer repair for oral and maxillofacial soft tissue defects." Pathology results: (nasal dorsum) invasive epithelial nests with significant atypia, frequent mitosis, and partial necrosis were observed, consistent with odontogenic ghost cell carcinoma based on history.
On September 20, 2024, the patient presented with a mass in the left nasal cavity and orbit. MRI indicated abnormal signals in the left nasal cavity, left periorbital, and lacrimal gland regions, suggesting recurrence and metastasis. The patient was admitted to our hospital for heavy ion therapy.
**Past Medical History:**
The patient is generally healthy, with no history of hypertension, diabetes, or other chronic diseases.
**Specialized Examination:**
No significant enlargement of superficial lymph nodes. A mass was observed on the left nasal dorsum, extending to the left supraorbital region and left nasal cavity. The left nasal dorsum was swollen, tender, smooth, and poorly mobile. Left nasal cavity touch bleeding (+). Left facial pain, purulent discharge, and tearing from the left eye were noted.
**Diagnosis:**
- Odontogenic ghost cell carcinoma of the left maxilla
- rpT2N1M0, Stage IVB
- KPS score: 80
**Heavy Ion Therapy Plan:**
1. **Target Delineation:**
- GTV: MRI-indicated irregular nodules and masses in the left nasal cavity, nasopharynx, oropharynx, left maxillofacial region, periorbital area, and nasal root, including surrounding invaded tissues. A 0.5 cm margin was added to form PTVboost.
- CTV: High-risk areas based on GTV, with appropriate cropping in the right eye and right optic nerve. A 0.3 cm margin was added to form PTV1.
- GTVnd_R: Enlarged lymph nodes in the right neck level II.
- GTVnd_L: Enlarged lymph nodes in the left neck levels Ib and II.
- CTVnd_R: Lymph node drainage area in the right neck level II.
- CTVnd_L: Lymph node drainage area in the left neck levels Ib-II.
A 0.3 cm margin was added to form PTVnd_R and PTVnd_L.
2. **Prescription Dose:**
- PTVboost: 8 Gy(RBE)/2 fractions
- PTV1, PTVnd_R, PTVnd_L: 64 Gy(RBE)/16 fractions
- Total dose to the tumor area: 72 Gy(RBE)/18 fractions
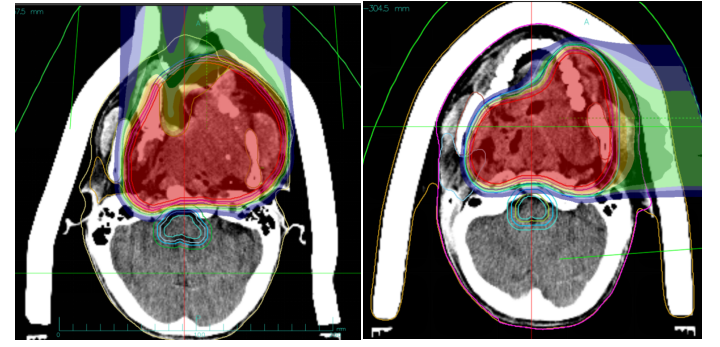
Figure 1: The total dose to the tumor region reached 72 Gy (RBE).
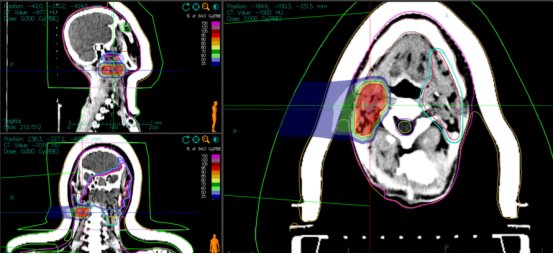
Figure 2: PTVnd_L 64 Gy (RBE)/16 fx.
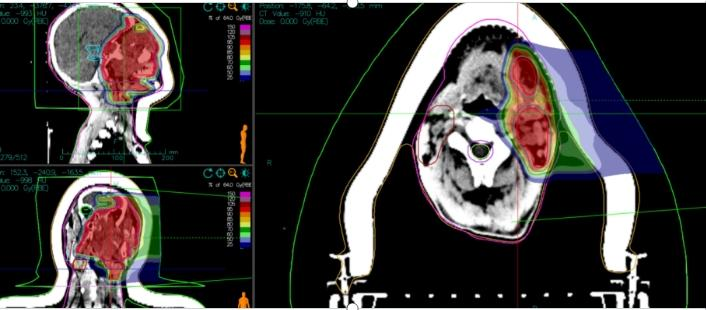
Figure 3: PTVnd_R 64 Gy (RBE)/16 fx, with the total dose to the tumor region reaching 72 Gy (RBE).
Efficacy Evaluation: The patient has completed carbon ion therapy. A follow-up MRI of the sinuses and neck showed that the multiple irregular nodules and masses in the left nasal cavity, left maxillofacial region, periorbital area, and nasal root have significantly reduced in size compared to before treatment. The tumor response is evaluated as Partial Response (PR).
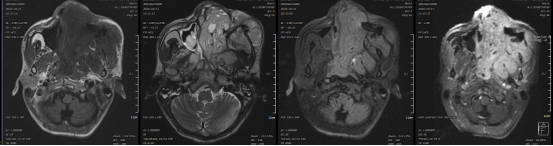
Figure 4: Before treatment: Multiple irregular nodules and masses were observed in the left nasal cavity, nasopharynx, oropharynx, left maxillofacial region, periorbital area, and nasal root, with extensive invasion of the left parapharyngeal and maxillofacial muscles.
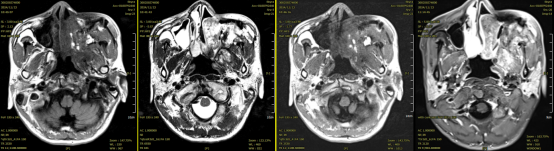
Figure 5: After treatment: Multiple irregular nodules and masses in the left nasal cavity, left maxillofacial region, periorbital area, and nasal root, with localized invasion of the left parapharyngeal and maxillofacial muscles, have shown a reduction in size compared to previous imaging.
During the course of carbon ion therapy, the patient developed acute grade 1 radiation-induced oral mucositis and acute grade 1 radiation-induced skin reaction after the 7th treatment session. Management included the use of mouthwash for rinsing, oral care, and the application of epidermal growth factor solution to promote skin healing. Following the 9th treatment session, the patient experienced acute grade 2 radiation-induced oral mucositis, which was managed with continued use of mouthwash for rinsing and oral care. Additional supportive treatments included pain relief, sleep regulation, and nutritional support. All symptoms resolved within two weeks after the completion of the treatment.
Discussion: Ghost cell odontogenic carcinoma (GCOC) is a rare malignant tumor of the jaw, with some cases arising de novo and others developing from pre-existing calcifying odontogenic cysts or ghost cell odontogenic tumors. GCOC most frequently occurs in the maxilla, accounting for 67% of cases, with a median age of onset at 40 years and a male predominance (2:1). It has a higher incidence among Asian populations. The tumor grows invasively without a distinct capsule, and its cut surface appears grayish-white, often accompanied by bone infiltration. Clinically, GCOC typically presents as swelling in the maxillofacial region, loosening and loss of teeth in the affected area, significantly impacting the patient's quality of life. Due to its diverse growth patterns and invasive nature into surrounding tissues, GCOC poses considerable treatment challenges. Although surgical resection is the primary treatment modality, the recurrence rate is high, particularly in cases with incomplete resection. Heavy ion therapy, with its precise targeting and high-energy deposition, allows for accurate irradiation of the tumor site, effectively reducing the risk of recurrence. Studies have shown that, compared to conventional radiotherapy, heavy ion beams have a relative biological effectiveness (RBE) of approximately 1.5 to 3 times, meaning they can more effectively damage the DNA of cancer cells, rendering them incapable of repair and leading to cell death.
