A Case Report of Carbon Ion Radiotherapy for Lacrimal Sac Tumor
A Case Report of Carbon Ion Radiotherapy for Lacrimal Sac Tumor
Hu Tingchao1, Zhang Yaoling1*, Wang Xinlan1, Zhang Tian'e1, Ma Shuping1, Tong Zongze1
Affiliations: Department of Heavy Ion Therapy, Wuwei Cancer Hospital, Gansu Province, China
Abstract
Background and Purpose: Lacrimal sac tumors are rare and highly invasive, with the majority being primary tumors. The etiology is not fully understood, but some are associated with chronic inflammation of the lacrimal gland. The most common type is lacrimal gland epithelial carcinoma, accounting for about 10% of orbital tumors. This study reports a case of carbon ion radiotherapy for a patient with moderate to poorly differentiated squamous cell carcinoma of the right lacrimal sac, focusing on the safety and efficacy of the treatment.
Case Presentation: A 45-year-old female patient presented with a round mass about the size of a mung bean at the root of the right nostril, accompanied by tearing. There was no redness, swelling, pain, significant secretion, visual impairment, headache, nausea, vomiting, orbital pain, diplopia, or visual distortion. The diagnosis was confirmed by orbital MRI, endoscopic biopsy of the right lacrimal sac tumor, and PET-CT.
Treatment:The patient underwent carbon ion radiotherapy with a total dose of 64 Gy (RBE) in 16 fractions, starting on July 20, 2022, and ending on August 12, 2022. Concurrently, she received four cycles of cetuximab weekly targeted therapy and two cycles of chemotherapy with albumin-bound paclitaxel 300 mg on day 1 and cisplatin 30 mg on days 1-2, 40 mg on day 3.
Clinical Outcome:The treatment was effective, with a partial response (PR) at the end of radiotherapy and 3 months post-treatment, and a complete response (CR) at 2 years post-treatment. The acute radiation skin injury grade was 1 according to RTOG criteria, and the adverse event grade was 1 according to CTCAE-V5.0. No ocular toxicity, such as vision loss or visual impairment, was observed 2 years after radiotherapy.
Conclusion: This case demonstrates the potential of carbon ion radiotherapy in treating lacrimal sac tumors, with favorable safety and efficacy profiles. The high relative biological effectiveness (RBE) of carbon ions allows for effective tumor cell killing with reduced damage to surrounding normal tissues.
Keywords: Lacrimal Sac Tumor; Carbon Ion; Radiotherapy
Introduction: Lacrimal sac tumors are a rare but highly aggressive type of tumor, commonly found in the lacrimal sac and lacrimal gland regions. The majority are primary tumors, and their etiology remains incompletely understood. A small number of cases are closely associated with chronic inflammation of the lacrimal gland, with lacrimal gland epithelial carcinoma being the most common, accounting for approximately 10% of orbital tumors. These tumors pose a significant threat to patients' health and lives[1]. Currently, a multidisciplinary approach involving eye-preserving surgery combined with postoperative radiotherapy and chemotherapy is typically employed to maximize the preservation of ocular function while controlling the tumor. [2-3]Radiotherapy plays a crucial role in the local treatment of both postoperative and non-surgical patients. Common postoperative radiotherapy techniques include photon external beam radiotherapy[4], brachytherapy, and proton external beam radiotherapy[5-6]. Although photon radiotherapy effectively controls tumors, it causes significant damage to surrounding normal tissues, potentially leading to severe complications such as vision loss. Carbon ions have a smaller penumbra and a narrower Bragg peak[7] compared to protons, making them more suitable for small and superficially located lacrimal sac and gland tumors. The relative biological effectiveness (RBE) of carbon ion radiotherapy is higher, meaning that at the same dose, carbon ions have a stronger tumor-killing effect. Currently, there are limited clinical studies on carbon ion radiotherapy for lacrimal sac malignancies, but existing research suggests that carbon ion radiotherapy has potential advantages in local control rates and survival rates. Therefore, this study analyzes the efficacy of carbon ion radiotherapy in a case of lacrimal sac malignancy, providing a reference for the potential dosimetric and biological advantages of this treatment approach.
Clinical Data:
General Information: A 44-year-old female patient presented with a round mass about the size of a mung bean at the root of the right nostril, accompanied by tearing. There was no redness, swelling, pain, significant secretion, visual impairment, headache, nausea, vomiting, orbital pain, diplopia, or visual distortion. The diagnosis was confirmed by orbital MRI, endoscopic biopsy of the right lacrimal sac tumor, and PET-CT.
Treatment Plan Implementation:The carbon ion radiotherapy plan involved the patient lying in a supine position, fixed with a vacuum bag and thermoplastic film. CT and MRI images were fused to delineate the target volume. The gross tumor volume (GTV) included the visible right lacrimal sac lesion on enhanced T1-weighted images. The clinical target volume (CTV) encompassed the GTV, right medial rectus muscle, right ethmoid sinus, and right maxillary sinus. Planning target volume 1 (PTV1) was the GTV + 0.3 cm, and PTV2 was the CTV + 0.3 cm. The prescribed dose was 64 Gy (RBE) in 16 fractions for PTV1 and 56 Gy (RBE) in 14 fractions for PTV2. Organs at risk (OAR) dose constraints were as follows: right eye: mean dose ≤ 30 Gy (RBE), right lens: left eye: maximum dose ≤ 9 Gy (RBE), brainstem: maximum dose ≤ 54 Gy (RBE), right optic nerve: 50% isodose line ≤ 56 Gy (RBE), right temporomandibular joint: mean dose ≤ 35 Gy (RBE), optic chiasm: maximum dose ≤ 54 Gy (RBE), left eye: mean dose ≤ 35 Gy (RBE), left lens: maximum dose ≤ 0 Gy (RBE).
Efficacy and Adverse Event Evaluation: Efficacy was assessed using the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1, and acute radiation toxicity was evaluated using the RTOG acute radiation injury grading system. Adverse events were graded according to CTCAE version 5.0.
Results: The treatment was effective, with a partial response (PR) at the end of radiotherapy and 3 months post-treatment, and a complete response (CR) at 2 years post-treatment. The acute radiation skin injury grade was 1 according to RTOG criteria, and the adverse event grade was 1 according to CTCAE-V5.0. No ocular toxicity, such as vision loss or visual impairment, was observed 2 years after radiotherapy.
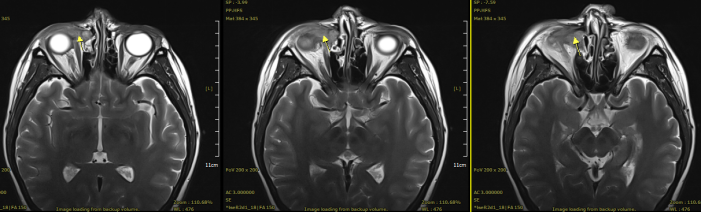
Figure 1: Pre-treatment (16mm × 22mm × 28mm)
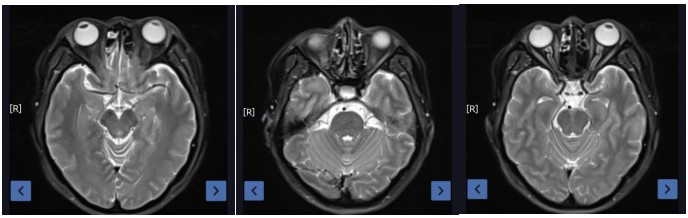
Figure 2: Post-treatment at 2 years (complete resolution of the lesion)
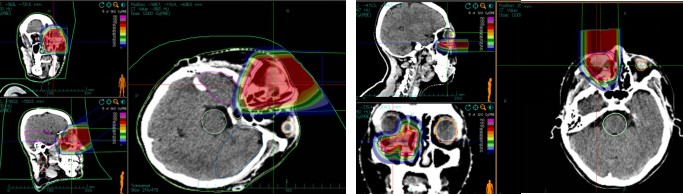
Figure 3: First course horizontal field: Prescription dose PTV 56 Gy (RBE)/14 fx; Second course vertical field: Prescription dose PTV = 8 Gy (RBE)/2 f.
Table 1: Efficacy Evaluation
| Time | Baseline Period | EOT | 3 Months after Treatment | 2 Years after Treatment |
|---|---|---|---|---|
| Maximum Diameter (mm) | 28 | 16 | 14 | CR |
| Efficacy Evaluation | PR | PR | CR |
Table 2: Acute Toxic Reactions
| Acute Toxic Reaction and Adverse Event | ||||||
|---|---|---|---|---|---|---|
| Acute Toxic Reaction | Classification | Time of Occurrence | Duration | |||
| G1 | G2 | G3 | G4 | |||
| Skin | √ | 2022-07-12 | 2 months | |||
| Radiation Therapy-Related Adverse Events | 分级 | Radiotherapy-Related | Time of Occurrence | |||
| G1 | G2 | G3 | G4 | |||
| Eye Injury | √ | Most likely related | Treatment - End of Treatment | |||
| Epistaxis | √ | Most likely related | Treatment - End of Treatment | |||
Conclusion
Carbon ion therapy, as a treatment for lacrimal sac tumors, is safe, effective, and demonstrates significant short-term efficacy
Discussion
Carbon ion radiotherapy, as a novel radiotherapy technique, has demonstrated significant dosimetric advantages and potential clinical efficacy in the treatment of lacrimal sac malignancies. It can significantly improve local control rates and overall survival while reducing treatment-related adverse effects.[8] In one study, patients with ocular tumors treated with carbon ion radiotherapy achieved 3-year overall survival, disease-free survival, and local control rates of 88.2%, 84.8%, and 94.7%[9], respectively. Additionally, the incidence of glaucoma post-treatment was low, indicating that carbon ion therapy has certain advantages in avoiding severe complications. A study by Skinner[10] et al. Summarized follow-up data from 46 patients with epithelial malignancies of the lacrimal apparatus, finding that those treated with carbon ion therapy retained ocular function while significantly reducing the occurrence of acute and long-term radiotherapy-related adverse effects. Research by Mizoe and other researchers showed that carbon ion therapy in head and neck malignancies significantly improved local control rates without increasing acute adverse effects. Therefore, carbon ion therapy for lacrimal sac and gland tumors may offer both dosimetric and biological advantages. Future research will further explore the optimal application of carbon ion radiotherapy in the treatment of lacrimal sac malignancies, as well as its combination with other therapeutic modalities, aiming to enhance treatment efficacy and patients' quality of life.
References
[1] Mohite A, Jenyon T, Manoj B, et al. Pseudodacryocystitis: paediatric case series of infected atypical ethmoid air cells masquerading as recurrent dacryocystitis. Eye (Lond). 2017; 31(4): 657-660. doi:10.1038/ eye. 2016. 282
[2] Woo KI, Kim YD, Sa HS, et al. Current treatment of lacrimal gland carcinoma. Curr Opin Ophthalmol. 2016;27(5):449-456.
[3] Shields JA, Shields CL, Epstein JA, et al. Review: primary epithelial malignancies of the lacrimal gland: the 2003 Ramon L. Font lecture. Ophthalmic Plast Reconstr Surg. 2004;20(1):10-21. doi:10.1097/01.IOP.0000103003.87842.BB
[4] Esmaeli B, Yin VT, Hanna EY, et al. Eye-sparing multidisciplinary approach for the management of lacrimal gland carcinoma. Head Neck. 2016;38(8):1258-1262. doi:10.1002/hed.24433
[5] Shields JA, Shields CL, Freire JE, et al. Plaque radiotherapy for selected orbital malignancies: preliminary observations: the 2002 Montgomery Lecture, part 2. Ophthalmic Plast Reconstr Surg. 2003;19(2):91-95. doi:10.1097/01.IOP.0000056020.66654.33
[6] Holliday EB, Esmaeli B, Pinckard J, et al. A Multidisciplinary Orbit-Sparing Treatment Approach That Includes Proton Therapy for Epithelial Tumors of the Orbit and Ocular Adnexa. Int J Radiat Oncol Biol Phys. 2016;95(1):344-352. doi:10.1016/j.ijrobp.2015.08.008
[7] Qu Jie, Tian Zhen, Wu Tiantian, et al. Research Progress on Lacrimal Sac Tumors [J]. Journal of Clinical Ophthalmology, 2022, 30(04): 379-383.
[8] Skinner HD, Garden AS,Rosenthal DI,et al. Outcomes of malignant tumors of the lacrimal apparatus: the University of Texas MD Anderson Cancer Center experience. Cancer. 2011;117(12):2801-2810. doi:10.1002/cncr.25813
[9] Nobutaka,Mizoguchi,Hiroshi,Tsuji,Shingo,Toyama,Tadashi,Kamada,Hirohiko,Tsujii,Yuko,Nakayama,Atsushi,Mizota,Yoshitaka,Ohnishi,Working Group for Ophthalmologic Tumors.Carbon-ion radiotherapy for locally advanced primary or postoperative recurrent epithelial carcinoma of the lacrimal gland.[J].Radiotherapy and oncology : journal of the European Society for Therapeutic Radiology and Oncology,2015,114(3):373-7
[10] Mizoe JE, Tsujii H, Kamada T, et al. Dose escalation study of carbon ion radiotherapy for locally advanced head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2004;60(2):358-364. doi:10.1016/j.ijrobp.2004.02.067

