A Case Report of Nasal Sinus Chordoma
A Case Report of Nasal Sinus Chordoma
A 54-year-old male presented with right nasal congestion, bleeding, and left eye pain. In December 2022, he underwent surgical treatment, and postoperative pathology confirmed chordoma. On January 8, 2023, an oculomotor nerve MRI revealed compression of the left oculomotor nerve origin by the left posterior cerebral artery PI, indicating tumor recurrence. Surgery was not feasible, and the patient experienced blurred vision, diplopia, and unsteady gait. He was admitted for carbon ion radiotherapy. The target dose for carbon ion therapy at our hospital was as follows:
- First course: Spot scanning was used for treatment. The prescribed dose for PTV was 39.0 Gy (RBE) in 13 fractions.
- Second course: The target area was divided into PTVboost1 (scattering) and PTVboost2 (spot scanning), with both fields irradiated simultaneously. The prescribed dose for PTVboost was 30.0 Gy (RBE) in 10 fractions.
- Total prescribed dose for the tumor region: 69.0 Gy (RBE) in 23 fractions.
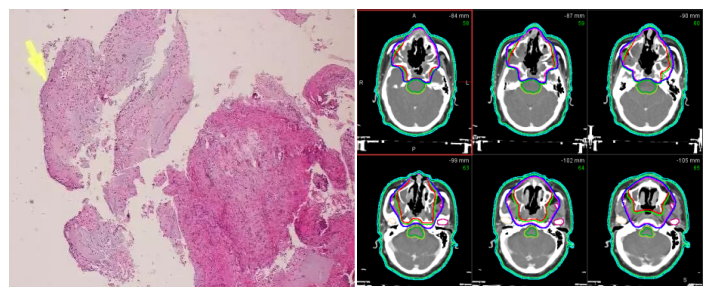
Figure 1 Pathology Figure 2 Target Delineation
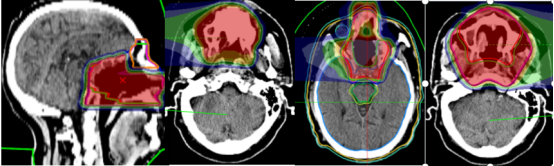
Figure 3: Target Field Design
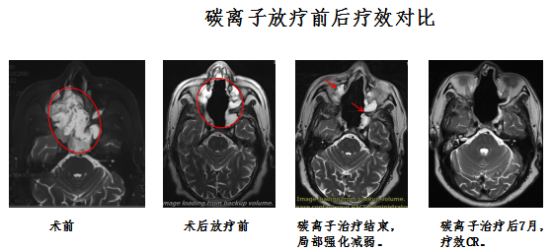
Figure 4: Carbon Ion Radiotherapy Comparison
The patient is currently in stable condition with no recurrence or metastasis.
Discussion:
Chordoma is a locally invasive or malignant tumor, commonly involving the clivus and sacrococcygeal region as an extradural tumor. It arises from embryonic remnants or ectopic notochord. These tumors can occur at any location along the axial spine but are most frequently found in the rostral clivus and sacrococcygeal region. The notochord is a degenerated structure in humans and other higher vertebrates. Although chordomas grow slowly and rarely metastasize distantly (though late-stage metastasis can occur), they are highly locally destructive. Due to their continued growth and potential harm to the body, as well as their high recurrence rate after surgery, they are classified as malignant tumors. Chordomas are rare, accounting for 1% to 4% of primary malignant bone tumors, and are more common in males.
Chordomas are most commonly found in middle-aged and elderly individuals aged 40 to 60, though they can occasionally occur in children and young adults. These tumors predominantly occur at the two ends of the spine, namely the skull base (35%) and the sacrum (50%), with the remaining 15% found in other vertebral bones. Occurrences outside the axial skeleton are rare, such as in the transverse processes of vertebrae or the nasal sinuses. Pain in the sacrococcygeal region is often the initial symptom. Most spinal chordomas are diagnosed after patients have experienced related symptoms for several months to years. The clinical manifestations depend on the tumor's location:
- Tumors in the occipital and sphenoid regions can cause headaches and symptoms related to cranial nerve compression (most commonly the optic nerve). Destruction of the pituitary gland may lead to pituitary dysfunction. Lateral or inferior extension can form a mass in the nasopharynx, obstructing the nasal cavity and resulting in purulent or bloody discharge.
- Tumors occurring at the lower clivus and the craniocervical junction often present with headaches and pain in the occipital or occipitocervical region, which may worsen with changes in head position.
The treatment options for chordoma include:
1. Surgery: The preferred approach is wide or complete resection.
2. Postoperative radiotherapy: Administered for cases with positive margins or residual tumor after surgery.
3. Radiotherapy target area: Chordoma is a low-grade malignant tumor. The CTV should be determined based on clinical examination and imaging, extending 0-10 mm from the GTV or targeting the postoperative tumor bed.
Radiation dose: 66-78 Gy, delivered at 2 Gy per fraction.
Heavy ions are high-LET (linear energy transfer) radiation, with energy deposition concentrated at the end of their range and minimal lateral scattering, resulting in sharp dose edges, which facilitates precise treatment (on the millimeter scale). Additionally, heavy ions exhibit a higher biological effectiveness, are independent of the cell cycle, and induce cell death through multiple mechanisms. They also have a lower oxygen enhancement ratio. Compared to conventional radiation therapy, heavy ion therapy offers significant advantages for treating radiation-resistant tumors. The dual benefits of heavy ions—dose depth distribution and biological effectiveness—significantly enhance the killing effect on tumor cells, thereby improving local tumor control rates. This makes heavy ion therapy a potentially valuable option for treating chordoma.
Radiotherapy Department Five: Hu Tingchao, Wang Xinlan, Zhang Yaoling, Ma Shuping, Zhang Tian'e, Tong Zongze.
