Is Higher Blood Flow Rate Always Better? Essential Truths for Hemodialysis Patients
Is Higher Blood Flow Rate Always Better? Essential Truths for Hemodialysis Patients
In hemodialysis treatment, blood flow rate (the speed at which blood passes through the dialyzer) is an indicator often noticed by patients and their families. Some believe that "a higher blood flow rate leads to better dialysis result," but is this really true? Today, let's discuss this topic to help hemodialysis patients scientifically understand the "balance" of blood flow rate.
Why is blood flow rate important?
Blood flow rate is one of the important parameters for measuring dialysis adequacy. It directly affects toxin clearance rate, water removal efficiency, and treatment safety. Both excessively high and low blood flow rates can pose risks:
● Sufficiently high blood flow rate: Helps remove toxins and excess water from the body more efficiently.
● Insufficient blood flow rate: May lead to inadequate dialysis, affecting treatment effectiveness.
But is the view that "higher is always better" truly scientific?
Potential risks of excessively high blood flow rate
1.Increased risk of low blood pressureExcessively high blood flow rate can accelerate blood withdrawal from blood vessels, potentially causing a sudden drop in blood pressure, leading to dizziness, nausea, or even shock. 34
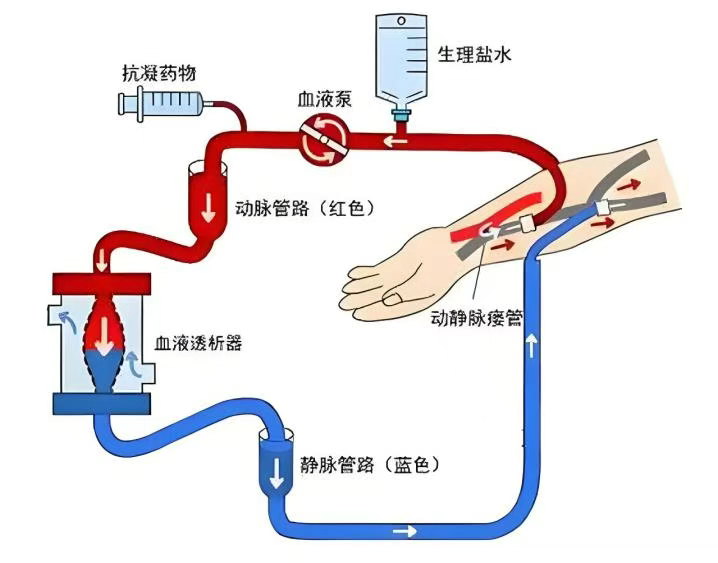
2.Vascular access damageLong-term high blood flow may exacerbate vascular endothelial injury, increasing the risk of thrombosis or stenosis, and affecting the lifespan of arteriovenous fistulas or grafts.
3.Increased burden on the heartFor patients with poor heart function, high blood flow may increase the cardiac load, potentially triggering issues like arrhythmias. 46
4.Increased risk of dialyzer clottingExcessively high blood flow may cause unstable blood flow velocity in the dialyzer, increasing the probability of clotting and reducing dialysis efficiency.
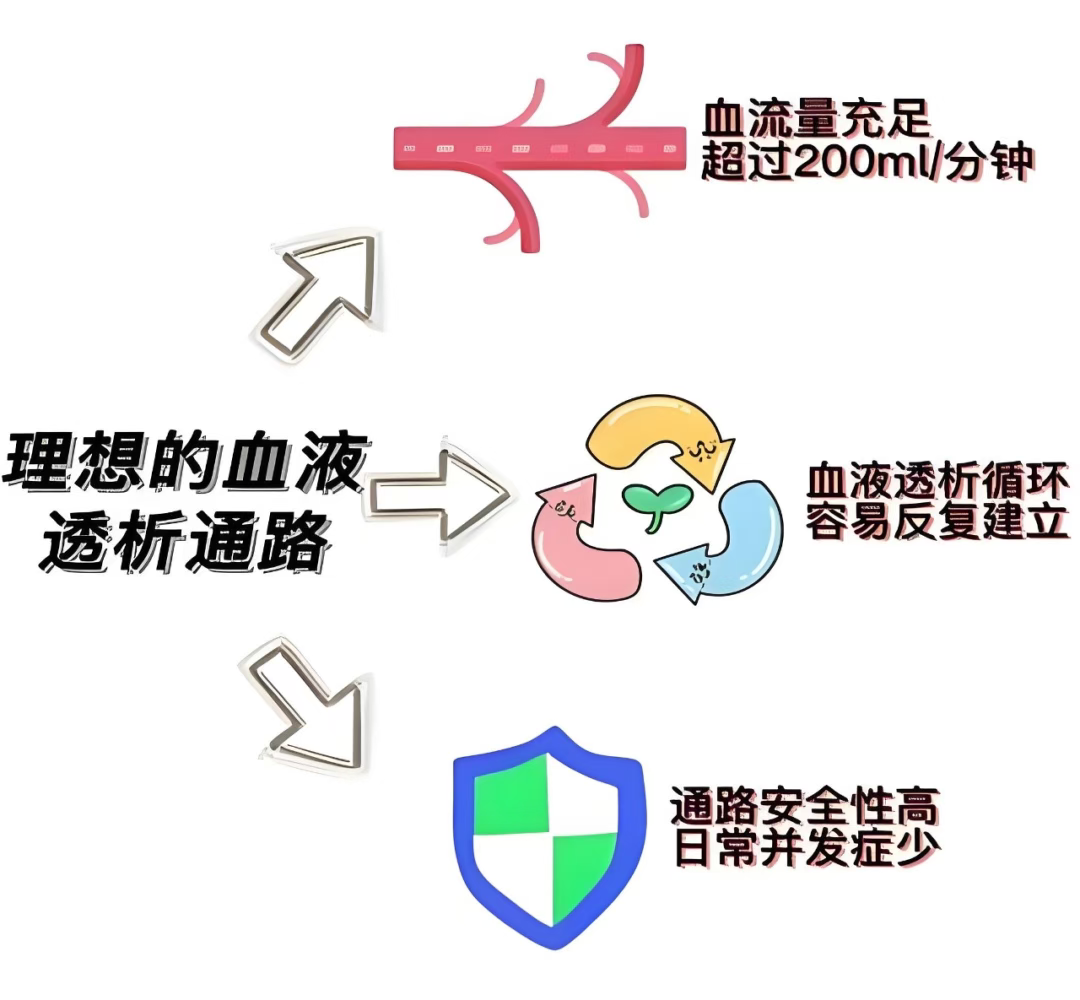
What is the reasonable range for blood flow rate?
● General recommendation: For adults, blood flow is typically controlled between 200-300 ml/min, and needs to be adjusted based on the individual patient's condition.
● Personalized adjustment: Doctors and nurses will comprehensively assess the patient's vascular condition, blood pressure, heart function, weight, and other indicators to set the most suitable blood flow rate.
Key principle:
"Adequate dialysis" ≠ "blindly pursuing high blood flow rate"Scientific blood flow rate should balance efficacy and safety, avoiding "pursuing high rates for their own sake."
How can patients cooperate in managing blood flow rate?
1.Regular monitoringCooperate with medical staff to monitor blood pressure, heart rate, and post-dialysis symptoms (such as dizziness, fatigue), and provide timely feedback on any abnormalities.
2.Avoid self-adjustment.Do not request an increase in blood flow rate due to concerns about "inadequate dialysis cleaning"; any adjustments should be made under professional guidance.
3.Improve vascular conditionProtect vascular access (e.g., arteriovenous fistula), avoid infection or thrombosis at the puncture site, and ensure smooth blood flow.
4.Reasonably control weightFollow medical advice to control weight gain between dialysis sessions, reducing blood volume fluctuations caused by excessive dehydration.
Summary: Adopt a scientific perspective on blood flow rate, safety in dialysis is key.
The setting of blood flow rate needs to be "tailored to the individual." Patients should not blindly pursue high or low values. Regular communication with the medical team to understand one's own physical condition and treatment parameters is essential for achieving safe and efficient dialysis treatment.
Final reminder
If you feel unwell during dialysis (such as dizziness, chest tightness), please inform the nurse immediately! Your comfort and safety are our utmost concern!
Wei Jinfen
Director of the Blood Purification Center, Department of Nephrology, Gansu Wuwei Cancer Hospital
Specialties: Acute/chronic kidney diseases due to various causes, such as acute/chronic nephritis, nephrotic syndrome, diabetic nephropathy, lupus nephritis, polycystic kidney disease, and liver diseases. Has unique insights into the management of temporary catheters, semi-permanent catheters, and internal fistulas in the hemodialysis center.
Expert Outpatient Clinic: Monday to Friday
Preliminary Review: Zhang Lihong
Final Review: Zhang Jie
