Analysis of Dose Decay at the Edge of Beam in Heavy Ion Radiotherapy
Analysis of Dose Decay at the Edge of Beam in Heavy Ion Radiotherapy
MA Xiao-yun ,ZHANG Yan-shan ,ZHANG Meng-ling ,MENG wan-bin ,LU Xiao-li (Wuwei Cancer Hospital ,wuwei 733000 ,China)
Abstract: [Objective] To analyze the dose decay at the edge of the beam under different incident modes and multiple dose segmentation Conditions during fixed beam irradiation using treatment planning system(TPS) ,so as to provide reference data for the relative safe distance between the target area and the organ at risk during heavy ion radiotherapy. [Methods] Uniform scanning mode was selected in heavy ion TPS ,and multiple heavy ion treatment plans with single beam irradiation ,two beams irradiation in opposite direction and two beams orthogonal irradiation under common segmentation conditions were designed in a homogeneous water phantom. The dose decay data of each plan was collected based on the position of the central axis of the edge of beam where the dose began to drop rapidly. [Results] The analysis of dose decay data showed that in the case of single beam irradiation ,the dose could drop to about 20% after 5mm distance from the back edge of the beam. When two beams were irradiated in opposite direction ,the dose could drop to about 50% in 5mm away from the posterior edge of the beam. In orthogonal irradiation of two beams ,the dose of posterior edge of the beam could drop to about 30~38% in a distance of 5mm. The dose drop at the back edge of the heavy ion beam center is rapid ,which is far better than X-ray. When designing the radiotherapy treatment plan ,the dose limit of organs at risk adjacent to the target region can reach the clinically acceptable range while achieve the dose of the target dose description. [Conclusions] Through the data analysis in the TPS ,it can be seen that the sharpness of the dose at the back edge of the heavy ion beam is better than that at the lateral edge ,but the generated X-ray pollution cannot be ignored. In practice ,the human body tissue is heterogeneous ,which will also affect the dose drop curve behind the field.Therefore ,the effect of uneven CT value on the dose drop of heavy ion beam should also be considered in Clinical treatment.
Subject words:heavy ion ;uniform scanning ;dose decay.
Heavy ions refer to ions with an atomic number greater than or equal to 2 that have lost their outer electrons. Heavy ions exhibit an inverted depth-dose distribution, known as the Bragg Peak. When charged heavy ions pass through human tissue, the dose curve remains relatively constant in the shallow regions, forming a low-dose plateau. However, at the end of their range, the ion velocity drops sharply, and the residual energy is completely released, forming a peak of high ionization density, known as the Bragg Peak. By adjusting the speed and intensity of heavy ions based on the shape and location of the tumor, the high-dose distribution region (Bragg Peak) can be precisely aligned with the tumor target area. This allows for three-dimensional conformal therapy, maximizing the destruction of tumor tissue while minimizing or almost completely sparing the surrounding normal tissue, thus providing effective protection. Additionally, compared to X-rays, heavy ions have a higher Relative Biological Effectiveness (RBE) in the Bragg Peak region, making them a superior form of radiotherapy[1]. This enables the killing of tumor cells in the target area while minimizing damage to the surrounding and irradiated normal tissues. Among heavy ions, carbon ions are considered the most suitable for clinical radiotherapy due to the largest difference in RBE values between the peak and plateau regions. When applied clinically for tumor radiotherapy, carbon ion therapy has minimal side effects, shorter treatment durations, and excellent efficacy, making it particularly suitable for treating certain solid tumors that are inoperable, resistant to conventional radiation, or recurrent after conventional radiotherapy. As of 2020, all heavy ion therapy systems used in clinical practice worldwide lacked rotating gantries and relied on fixed beam heads, typically designed for horizontal, vertical, and 45° angle directions. This allows for multiple irradiation methods for tumor lesions. Due to the unique physical advantages of heavy ions, physicists designing radiotherapy plans do not need to use 5–7 or more fields, as is common in X-ray radiotherapy, to adjust the target dose and limit the dose to critical organs. Heavy ion radiotherapy plans often require only 2–3 fields to meet clinical requirements. For fixed beam head treatments, single-field irradiation, two-field opposing irradiation, and two-field orthogonal irradiation are the most common. The individual Bragg Peak is sharp and narrow, only a few millimeters thick. To ensure that heavy ion beams can cover tumors of various sizes, there are two beam delivery methods: passive beam delivery, which uses a fixed Spread-Out Bragg Peak (SOBP), and active spot scanning. Uniform scanning is a passive beam delivery mode used in clinical heavy ion radiotherapy. It employs triangular wave scanning to laterally expand the beam and a ridge filter to longitudinally broaden the Bragg Peak, combined with a multi-leaf collimator for conformal irradiation in the lateral direction[2]. There is limited analysis of the dose fall-off at the edges of the target area formed by the unique Bragg Peak of heavy ions. Clinicians often need to consider the relationship between the tumor location and surrounding critical organs when treating patients with heavy ions to ensure that the target dose is achieved while meeting the dose limits for adjacent critical organs. This study, under the carbon ion uniform scanning mode, analyzes the dose fall-off rates at the target edges under various field arrangements and dose fractionation conditions. It provides reference data for clinicians treating patients with heavy ion radiotherapy and for delineating the relative safe distance between the target area and critical organs during contouring.
Ⅰ. Materials and Methods
1.1 Research Tool
The heavy ion planning system, version ciPlan1.0, is utilized as the research tool. The principle of this system is to use CT as the foundational input data, extracting CT values (Hounsfield Unit, HU). After converting the CT values along the beam path into water-equivalent values, a biological model is employed to calculate the range, energy deposition, and dose distribution of heavy ions in the human body or medium. The system relies on the programming language Microsoft Visual C++ to simulate the functional characteristics of equipment such as the accelerating electric field (accelerating ring), deflection, and focusing magnetic fields. It integrates the use of ridge filters and energy degraders to digitally control the beam spot size, nominal beam energy, and Bragg Peak spread. The collimator features a mortise-and-tenon structure with multi-media tungsten-copper alloy leaves, ensuring compatibility with the treatment terminal.
The built-in algorithm is based on the dose distribution characteristics of the Bragg Peak formed by high-energy carbon ion (12C6+) beams in water. Utilizing the Pencil Beam Calculation (PBC) principle, the system includes parameters such as treatment room gantry angle, energy levels, radial dose distribution of the beam, and a summary table of Relative Biological Effectiveness (RBE) ratios. It supports essential functions such as importing patient CT images, rigid image fusion and registration, delineation of target areas and normal organs, plan creation, plan data collection, plan comparison, plan report export, and verification plan generation.
1.2 Research Statistical Methods
A uniform cubic water phantom was set up in the heavy ion planning system, with a target area size of 10cm×10cm×10cm. Heavy ion plans were designed under various common fractionation conditions, including single-field irradiation, two-field opposing irradiation, and two-field orthogonal irradiation. After completing the plan design, the position and dose collection tools of the planning system were used to precisely collect lateral curve distribution data along the central axis of the radiation field. Dose variation data at the edge of the target area behind the radiation field were extracted. The position of the 95% isodose line at the rear edge of the central axis of the radiation field was used as the reference, defining its dose as 100% and the distance as 0 mm. Dose data at points within a 20 mm distance were collected. We collected dose fall-off data for uniform phantom standard plans with a total dose of 60GY (RBE), fractionated into 20, 15, 10, and 6 sessions1.
Ⅱ. Results
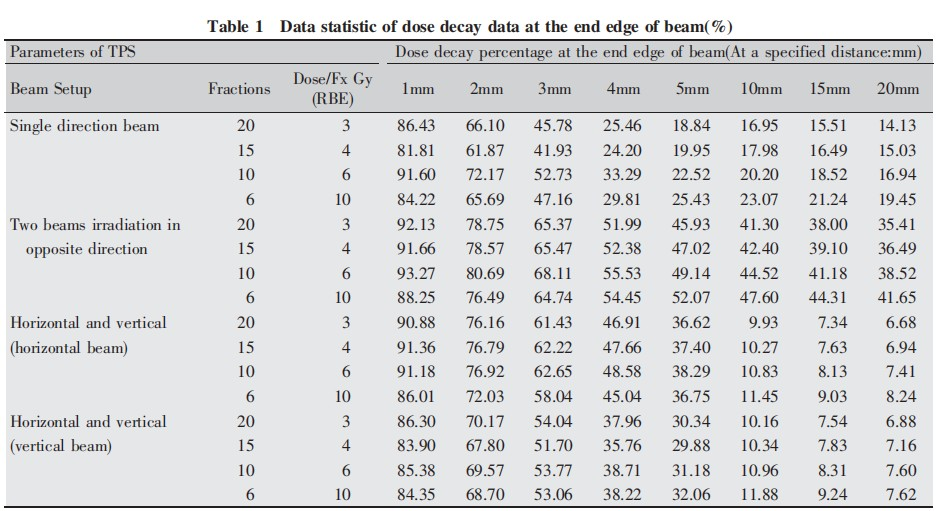
2.1 Relative Dose at a Certain Distance from the Rear Edge of the Radiation Field
The dose fall-off trends for the same irradiation method under different fractionation conditions were generally similar (Table 1). When using a single radiation field, the dose along the central axis behind the radiation field rapidly fell to approximately 50%–60% of the prescribed dose at a distance of 3 mm from the 95% isodose line. At a distance of 5 mm from the 95% isodose line, the dose fell to approximately 20%–30% of the prescribed dose. This allows for cases where critical organs are close to the target area in heavy ion therapy. When designing treatment plans, physicists can ensure that the target dose requirements are met while reducing the dose to adjacent critical organs to within the specified limits.
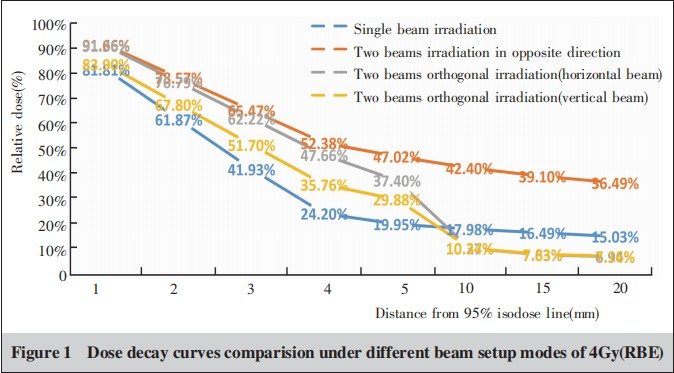
2.2 Dose Fall-Off Curves Under Different Field Arrangements
A single fraction of 4Gy (RBE) was selected in the planning system, and the dose curves of different field arrangements (Figure 1) were compared. From the figure, it can be observed that the dose fall-off is fastest in single-field irradiation, which intuitively reflects the steep dose drop behind the Bragg Peak, a characteristic of the two-dimensional conformal therapy in the heavy ion uniform scanning mode: conformal shaping at the posterior edge of the target area. The dose fall-off is slowest in two-field opposing irradiation. This is because the rear edge of one field in the two-field plan is the front edge of the other field. When heavy ion beams penetrate the object, the plateau doses of multiple Bragg Peaks overlap due to the Spread-Out Bragg Peak (SOBP), resulting in a relatively high dose at the front edge of the Bragg Peak after SOBP. Additionally, the dose in the two-field opposing plan remains at a relatively high level (greater than 35% at 20 mm) even after the fall-off, for the same reason.
In two-field orthogonal irradiation, the dose fall-off behind the field is intermediate. The rear edge of one orthogonal field is the lateral edge of the other field, and its dose is a superposition of the rear edge of the Bragg Peak and the penumbra of the dose edge. Compared to the fall-off at the rear edge of a single Bragg Peak, the fall-off is slightly slower, and the distance to the flat region is longer. After the steep fall-off, the dose curve becomes flat. In this flat region, the dose at the rear edge of the two-field orthogonal irradiation is lower than that of single-field irradiation. The X-ray contribution in this part forms a "tail" behind the Bragg Peak, creating a low-dose region posterior to the Bragg Peak. Due to the minimal lateral scatter of X-rays, such a low-dose region does not exist at the lateral edge of the field. In two-field orthogonal irradiation, the doses at the rear and lateral edges of the fields are superimposed. With a 1:1 weighting of the two fields, the dose in the low-dose region behind a single field is essentially twice that behind the two-field orthogonal irradiation.
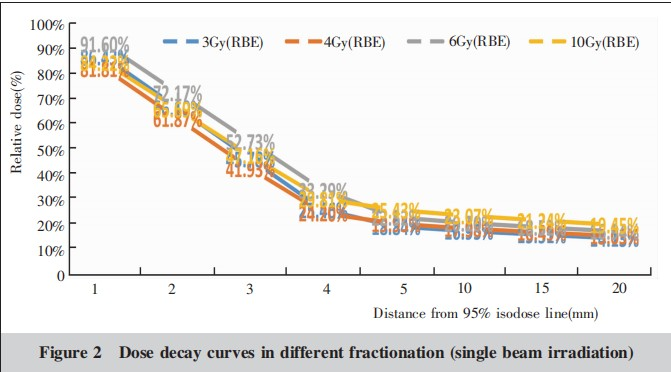
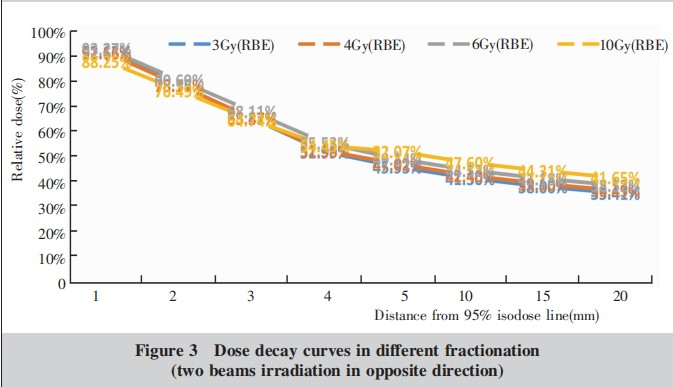
2.3 Dose Fall-Off Curves Under Different Fractionation Schedules
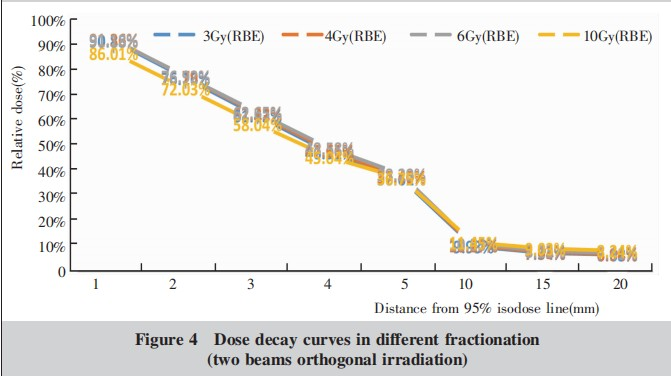
Comparative graphs of dose fall-off curves under different fractionation schedules were plotted for three irradiation methods: single-field irradiation, two-field opposing irradiation, and two-field orthogonal irradiation (Figures 2–4). It can be observed that the trends of the dose fall-off curves for the same irradiation method under different fractionation schedules are essentially the same. However, in the case of hypofractionation (single fraction of 10GY (RBE)), the overall dose is slightly higher, particularly more noticeable in single-field irradiation and two-field opposing irradiation.
Ⅲ. Discussion
Due to the physical characteristics of the Bragg Peak in heavy ions, the dose distribution at the edge of the target area exhibits a steep fall-off during radiotherapy compared to traditional X-ray therapy. This allows for better protection of surrounding critical organs. This advantage of heavy ions enables the treatment of target areas that are particularly close to critical organs. The purpose of this study is to analyze the dose fall-off gradient at the posterior edge of the target area in heavy ion radiotherapy, providing clinical reference data. When designing a heavy ion treatment plan, the choice of irradiation method generally depends on the location of surrounding critical organs. Selecting an appropriate beam angle can minimize the dose to normal organs.Beam delivery refers to the process of transporting heavy ion beams from the accelerator to the target area for irradiation. Its purpose is to shape the beam into the required irradiation field, ensuring that the patient's target area receives a uniform and sufficient dose while minimizing harm to healthy tissues. There are two types of heavy ion beam delivery methods: passive beam delivery, which uses a fixed Bragg Peak spread, and active spot scanning. In active beam delivery, the accelerator actively changes the particle energy to adjust the depth of ion beam penetration, while a magnetic scanning system guides the pencil beam for conformal or intensity-modulated irradiation of the tumor target area. During spot scanning treatment, to reduce the number of layered irradiations and shorten treatment time, the sharp Bragg Peak of a monoenergetic beam is appropriately broadened using a mini ridge filter, which transforms the Bragg Peak into a micro-broadened peak (mini-isoBP) with a Gaussian distribution.In passive beam delivery, the accelerator provides a fixed-energy beam, which is laterally expanded into a large irradiation field through scanning magnets and scatterers. The ridge filter longitudinally broadens the sharp peak of the monoenergetic beam to match the thickness of the tumor. A range shifter placed along the beam path adjusts the beam energy to achieve different penetration depths. A multi-leaf collimator is used to shape the irradiation field to conform to the projection contour of the tumor target area in the beam direction. The shape of the high-dose region at the posterior edge of the broadened Bragg Peak is adjusted by a tissue compensator placed on the patient's body surface, avoiding irradiation of critical organs behind the tumor target area.The data in this study were analyzed under the uniform scanning mode of passive heavy ion beam delivery. It can be observed that due to the unique physical properties of heavy ion beams, the dose fall-off at the edge of the target area is very rapid. At a distance of 5 mm from the 95% isodose line at the rear edge of the heavy ion beam, the dose can fall to approximately 20%–30% of the prescribed dose, meaning that 70%–80% of the dose is attenuated within 5 mm. This is a significant advantage of heavy ions, allowing for safe radiotherapy in cases where tumors are close to critical organs.In X/Y-ray radiotherapy, a study compared the dose fall-off gradients at the edge of the target area in stereotactic radiotherapy for pancreatic cancer using five devices: CyberKnife, TomoTherapy, Edge accelerator, Trilogy accelerator, and Gamma Knife. All five devices were able to meet clinical requirements for pancreatic cancer stereotactic radiotherapy, with CyberKnife and Gamma Knife exhibiting superior dose fall-off gradients[7]. In another study, the CyberKnife system was used to perform stereotactic body radiotherapy (SBRT) for vertebral metastases, and the relative dose fall-off speed in the spinal cord direction was analyzed. It was found that the relative dose fall-off was (0.87±0.60)mm/5%Dmax[8] for the 40 Gy group and (0.69±0.16)mm/5%Dmax for the 33 Gy group. These studies show that in X/Y-ray radiotherapy, stereotactic radiotherapy has a relatively fast dose fall-off, with CyberKnife and Gamma Knife exhibiting superior dose fall-off gradients of approximately 0.8 mm per 5% dose fall-off. However, heavy ion beams can attenuate 8%–19% of the dose within 1 mm at the rear edge of the field, making the dose fall-off of heavy ion beams significantly faster than that of X/Y-ray radiotherapy. This enables heavy ions to treat challenging cases where critical organs are very close to the target area. When designing treatment plans, physicists can ensure that the target dose requirements are met while reducing the dose to adjacent critical organs to within the specified limits.Since the data in this study were collected from a heavy ion treatment planning system using a uniform water phantom, it is important to note that in clinical practice, the human tissues traversed by heavy ion beams are heterogeneous. The planning system calculates doses based on CT values, and the heterogeneity of human tissues can affect the dose fall-off curve behind the irradiation field. Therefore, in actual heavy ion patient treatment, the values calculated by the planning system should be used as the benchmark. When delineating the target area, the relationship with adjacent critical organs should be carefully considered to ensure that the target area receives the prescribed dose while the dose to neighboring critical organs remains within clinically acceptable limits.Due to the high cost of heavy ion treatment systems, heavy ion radiotherapy is often used to treat tumors that have recurred after conventional radiotherapy or cases where tumors are too close to critical organs for conventional radiotherapy. Effectively and safely treating such patients is a challenge for heavy ion practitioners and physicists.
Reference
[1]夏文龙 ,胡伟刚 ,戴建荣,等.粒子治疗技术的进展[J]. 中华放射肿瘤学杂志 ,2017 ,26(8):951-955.
Xia WL ,Hu WG ,Dai JR ,et al. Progress in charged particle therapy[J]. Chinese Journal of Radiationoncology , 2017 ,26(8):951-955.
[2]戴中颖 . 重离子三维点扫描技术及相关重离子剂量学研 究[D]. 北京. 中国科学院研究生院 ,2012.1-112.
Dai ZY. Heavy ion 3D spot scanning technology and related heavy ion dosimetry[D]. Beijing:Graduate school of Chinese Academy of sciences ,2012.1-112.
[3] Mitsutaka Yamaguchi ,Chih一Chieh Liu ,Hsuan一Ming Huang , et al. Dose image prediction for range and width verifications from carbon ion-induced secondary electron bremsstrahlung x一rays using deep learning workflow[J]. Med Phys ,2020 , 47(8):3520-3532.
[4]康月航 ,盛尹祥子 ,赵静芳 ,等 .质子束流蒙特卡罗模型 的建立及对脊形滤波器的探究[J]. 中国医学物理学杂 志 ,2020 ,37(5):535-540.
kang YH ,shengyin XZ ,zhao JF ,et al. Monte carlo simulation of proton beams and investigation on ripple filters[J]. Chinese Journal of Medical physics ,2020 ,37(5):535-540.
[5]李小波 ,江柳清 ,吴晓东 ,等 . 高剂量格栅状放疗技术及应用[J]. 中华放射肿瘤学杂志 ,2018 ,27(6):624-628.
Li XB,Jiang LQ ,Wu XD ,et al. The application of high-dose grid radiotherapy technique [J]. Chinese Journal of Radiation Oncology,2018,27(6):624-628.
[6]盛尹祥子 ,Kambiz Shanazi,王巍伟 ,等. 点扫描质子束治疗机头的蒙特卡罗模拟和验证[J]. 中华放射医学与防护杂志 ,2019,39(8):635-640.
ShengYinXz ,KambizShanazi,WangWW,etal. Monte Carlo simulation and verification of a scanning proton beam nozzle[J]. chinese Journal of Radiological Medicine and protection,2019,39(8):635-640.
[7]上海医学会肿瘤放射治疗分会立体定向放疗学组 ,曹洋森 , 张建英 ,等 . 五种光子放疗设备在胰腺癌立体定向放疗中剂量学比较[J].中华放射肿瘤学杂志 ,2021 ,30(2) : 156-163.
Stereotactic radiotherapy group of Shanghai Medical Association,Cao YS,zhang JY ,et al. Comparison of dose distributions among five radiotherapy apparatuses in stereo tactic body radiation therapy for pancreatic cancer [J]. Chinese Journal of Radiation Oncology,2021,30(2):156-163.
[8]王金媛 ,鞠忠建 ,王小深 ,等. 椎体转移瘤立体定向放射治 疗剂量跌落梯度分析[J].中国医学装备,2015,(9):1-4 ,5.
WangJY, Ju ZJ, WangXS ,etal. The analysis of dose falling gradient in the treatment of spinal metastatic tumors implementing SBRT[J]. China Medical Equipment , 2015,(9) : 1-4 ,5.
