Clinical Observation of Abscopal Effect in Carbon Ion Therapy for Recurrent Thymic Carcinoma
Clinical Observation of Abscopal Effect in Carbon Ion Therapy for Recurrent Thymic Carcinoma: A Case Report
Zhang Yihe, Zhang Yanshan, Li Xiaojun, Pan Xin
Keywords: Carbon ion therapy, Abscopal effect, Bystander effect, Thymic carcinoma
DOI: 10.12354/j.issn.1000-8179.2021.20211145
The patient was a 43-year-old woman with no significant past medical history and no history of smoking or chronic lung disease. She presented to Wuwei Tumor Hospital in February 2009 with complaints of palpitations and dyspnea for 4 months. A chest CT scan revealed an occupying lesion in the anterior superior mediastinum, suspected to be a thymic tumor with possible invasion of the pericardium and left lung (Figure 1A). On February 16, 2009, she underwent an “extended resection of thymic tumor + partial resection of the left upper lobe of the lung, phrenic nerve, and pericardium.” Postoperative pathology showed: (anterior superior mediastinum) thymic non-keratinizing squamous cell carcinoma. The tumor had invaded the pericardium and lung but did not involve major blood vessels or lymph nodes. The pathological diagnosis was Masaoka stage IIIa, type C: thymic carcinoma. Postoperative chest CT indicated: post-thymic cancer surgery status, triangular fluid collection under the left sternum and anterior pericardial space effusion, extensive left pleural thickening and adhesions with a small amount of pleural effusion, localized bone defect at the sternum post-surgery, and soft tissue swelling (Figure 1B). The final postoperative diagnosis was pT3N0M0, stage IIIa, according to the American Joint Committee on Cancer (AJCC) 8th edition staging system. Thirty-five days after surgery, the patient received postoperative intensity-modulated radiotherapy (IMRT) with a total dose of 50 Gy delivered in 25 fractions, targeting the original tumor bed and the upper mediastinum. Thereafter, the patient did not receive any further treatment and was followed up regularly with chest CT scans. In December 2019, the patient again experienced palpitations and dyspnea. A follow-up chest CT showed multiple nodules in the left pleura, diaphragmatic crus, and peritoneum, with the largest lesion located near the pericardium in the left pleura, measuring 6.3 cm × 5.2 cm. Multiple small lymph nodes were also noted in the left supraclavicular root, mediastinum, and retroperitoneum, suggesting recurrent and metastatic thymic carcinoma. The clinical diagnosis was rcT2N2M1a, stage IVa. After multidisciplinary team (MDT) discussion, considering the patient’s long disease-free survival period following her previous surgery and radiotherapy, as well as the indolent biological behavior of the tumor, it was decided to administer palliative carbon ion radiotherapy only to the largest tumor near the pericardium in the left pleura, which was compressing and invading the heart, in order to alleviate the patient’s symptoms of palpitations and dyspnea. Carbon ion therapy was chosen due to its unique biological and physical advantages. Biologically, carbon ions exhibit higher linear energy transfer (LET) and greater relative biological effectiveness (RBE), along with a low oxygen enhancement ratio (OER) that is unaffected by tumor hypoxia, thereby improving local tumor control. Physically, the carbon ion beam features a Bragg peak and minimal lateral scatter, allowing for more precise dose distribution [1]. As a result, while delivering a high dose to the tumor, the radiation exposure to the heart and lungs could be minimized, thus sparing critical organs.
Treatment Plan:
The patient was positioned prone with her hands crossed over her head (left hand on top), a pillow under her forehead, and immobilized using a large vacuum cushion and thermoplastic mask. CT scans were performed with a slice thickness of 3 mm, including plain, contrast-enhanced, and 4D sequences. The CT images were transferred to the “rtStation” treatment planning system for target delineation.
Target Delineation:
• Gross Tumor Volume (GTV): The largest visible tumor adjacent to the left pericardium.
• Clinical Target Volume (CTV): GTV expanded by 5 mm.
• Planning Target Volume (PTV): CTV expanded by 5 mm.
Adjustments were made to spare critical organs; specifically, a 1 cm safety margin was maintained next to the left ventricle to protect it.
Treatment Regimen:
The carbon ion therapy plan was designed using the Ci-Plan planning software. The requirement was that 90% of the PTV receive the prescribed dose. A single left-side horizontal field plus one vertical field were used, delivering a total dose of 60 GyE to the lesion (Figure 2), with a single fraction dose of 4 GyE. Treatment was administered once daily, 5 days per week (Monday to Friday), for a total of 12 fractions (fx) over 3 weeks. The carbon ion dose was expressed in photon-equivalent dose (GyE), where GyE is defined as the physical dose multiplied by the RBE of carbon ions, typically set at 3.0 [2]. The patient did not receive any other treatments during or after radiotherapy.
Outcome:
After treatment, the patient’s symptoms of palpitations and dyspnea were relieved. During treatment, only mild skin pigmentation at the irradiated site occurred, classified as Grade 1 skin reaction according to the Radiation Therapy Oncology Group (RTOG) acute radiation injury grading criteria and as Grade 1 radiation dermatitis according to the Common Terminology Criteria for Adverse Events (CTCAE) version 5.0. The skin reaction had largely resolved two months after radiotherapy. A follow-up chest CT performed on the day after treatment completion showed not only shrinkage of the irradiated lesion (the largest lesion near the left pericardium) but also varying degrees of reduction in metastatic lesions in areas receiving low-dose or no radiation (left chest wall and left diaphragmatic crus), with continued shrinkage observed during the subsequent one-year follow-up (Figures 3A–3D). The maximum diameters of the lesions were as follows:
• Left pericardium lesion: 6.3 cm (pre-treatment), 4.6 cm, and 3.9 cm (at 1 year post-treatment).
• Left chest wall lesion: 2.8 cm, 1.9 cm, and 0.8 cm.
• Left diaphragmatic crus lesion: 4.1 cm, 3.9 cm, and 3.4 cm.
According to the RECIST 1.1 criteria for solid tumors, the efficacy was evaluated as a partial response (PR).
Due to the unique physical advantages of carbon ions, the doses received by critical organs such as the heart and lungs were kept low, providing better protection to normal tissues. Throughout the treatment, the patient did not experience any acute radiation injuries of Grade 2 or higher, demonstrating that this treatment approach was both safe and effective.
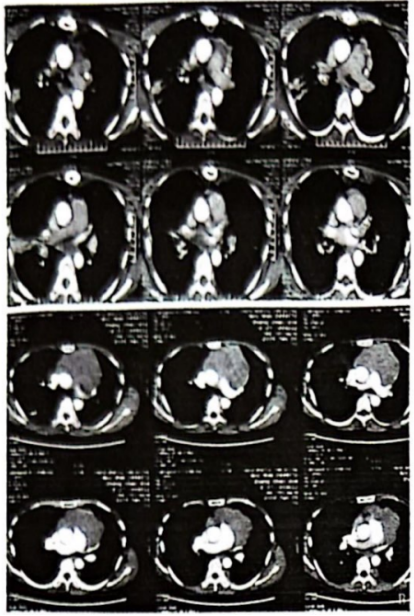
A: Preoperative contrast-enhanced chest CT (January 9, 2009); B: Postoperative contrast-enhanced chest CT (February 21, 2009)
Figure 1 Preoperative and postoperative images
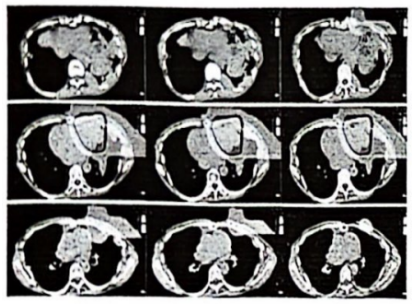
Figure 2 Beam directions and dose distribution cloud map on the treatment planning system (one left horizontal field + one vertical field)
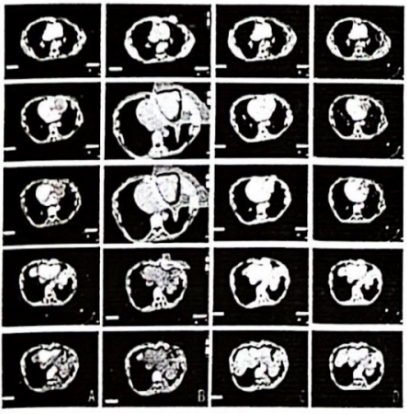
A: Before carbon ion therapy (March 24, 2020); B: 1%–110% dose cloud map; C: After carbon ion therapy (April 10, 2020); D: One year after carbon ion therapy (April 19, 2021); Red – target dose irradiation area; Green – low-dose irradiation area; Purple – non-irradiated area.
Figure 3 Imaging of chest lesions before and after treatment
Summary
The abscopal effect refers to the phenomenon where irradiation of a tumor target leads to the shrinkage or even disappearance of tumors in non-irradiated areas. Its mechanism may involve local radiotherapy not only directly killing tumor cells but also promoting the release of pro-inflammatory factors by immune cells, which act on non-irradiated tumor sites, inducing chromosomal breaks or mutations in tumor cells outside the irradiated field, thereby causing tumor shrinkage or disappearance. Additionally, it may involve the release of tumor-associated antigens and alterations in tumor cell phenotypes, triggering a systemic anti-tumor immune response that suppresses the growth of tumors outside the irradiated field to some extent. The occurrence of the abscopal effect may be related to the induction of an in situ tumor vaccine by radiotherapy. The in situ vaccine effect refers to the phenomenon where radiotherapy triggers acquired immune responses and specific antigen presentation reactions against tumor-associated antigens at the irradiated site. Sharabi et al. [3] reported that a single high-dose radiotherapy can enhance the antigen presentation of tumor-associated antigens and T-cell recognition, making it easier to induce the abscopal effect. This may be related to the sensitivity of different tumors to radiation, the characteristics of the radiation itself, the single radiation dose, and whether it is combined with other treatments. The abscopal effect has been observed in various types of tumors, particularly in reports where conventional radiotherapy combined with immunosuppressive agents induced the abscopal effect, including malignant lymphoma, liver cancer, cervical cancer, melanoma, and colorectal cancer. However, there are very few case reports of the abscopal effect being continuously observed in patients with postoperative recurrent and metastatic thymic carcinoma after standalone carbon ion radiotherapy and during follow-up. In this case, the abscopal effect induced by carbon ion therapy persisted until the last observation, one year after the end of treatment. The non-irradiated tumors shrank immediately after the completion of carbon ion therapy without receiving any other treatments and continued to shrink during subsequent follow-up, which could be clearly observed on enhanced CT scans. Nevertheless, the mechanism by which non-irradiated tumors elicit immune enhancement remains unclear. The combination of immune checkpoint inhibitors with radiotherapy has been shown to increase the incidence of the abscopal effect. However, in this case, the patient did not receive any immunotherapy or other drug treatments, and the abscopal effect was entirely attributed to carbon ion therapy. Whether the abscopal effect from standalone carbon ion therapy is due to the tumor's inherent sensitivity to radiation, the uniqueness of the patient's immune system, or the distinctive physical and biological advantages of carbon ions is difficult to distinguish. It is also unclear whether this mechanism is related to the abscopal effect observed with photon irradiation and whether it can be further enhanced by combining with immunotherapy, which requires further investigation.
References
[1] Masashi K, Yusuke D, Junichi S, et al. Multicenter study of carbon-ion radiation therapy for mucosal melanoma of the head and neck: subanalysis of the Japan carbon-ion radiation oncology study group (J-CROS) study (1402 HN)[J]. Int J Radiat Oncol Biol Phys, 2018, 102(2):353-361.
[2] Kanai T, Endo M, Minohara S, et al. Biophysical characteristics of HIMAC clinical irradiation system for heavy-ion radiation therapy[J]. Int J Radiat Oncol Biol Phys, 1999, 44:201-210.
[3] Sharabi AB, Nirschl CJ, Kochel CM, et al. Stereotactic radiation therapy augments antigen-specific PD-1-mediated antitumor immune responses via cross-presentation of tumor antigen[J]. Cancer Immunol Res, 2015, 3(4):345-355. DOI: 10.1158/2326-6066.CIR-14-0196
Preliminary Review: Liu Wenyu
Secondary Review: Zhang Jie
