3D-CRT versus IMRT for Cervical Cancer: Efficacy and Effects on Serum CYFRA 21-1, CEA, and SCC Antig
Efficacy of 3D Conformal Radiotherapy versus Intensity-Modulated Radiotherapy for Cervical Cancer and Impact on Serum Levels of CYFRA 21-1, Carcinoembryonic Antigen, and Squamous Cell Carcinoma Antigen
Zhang Zhichao, Chen Dongji
(Department of Radiotherapy, Gansu Wuwei Cancer Hospital, Wuwei, Gansu 733000, China)
【Abstract】 Objective To observe the efficacy of three-dimensional conformal radiotherapy (3D-CRT) versus intensity-modulated radiotherapy (IMRT) in treating cervical cancer, and to analyze changes in serum levels of cytokeratin 19 fragment (CYFRA21-1), carcinoembryonic antigen (CEA), and squamous cell carcinoma antigen (SCCA). Methods A total of 82 cervical cancer patients admitted to Gansu Wuwei Cancer Hospital between June 2020 and June 2023 were selected as subjects and randomly divided into a control group and an observation group, with 41 cases in each group. The control group received 3D-CRT, while the observation group received IMRT. Clinical efficacy, radiation doses to the femur, rectum, small intestine, bladder, and bone marrow, levels of CYFRA21-1, CEA, SCCA, and T lymphocyte subsets, as well as complications, were compared between the two groups. Results There was no statistically significant difference in overall efficacy or total effective rate between the two groups (all P>0.05). The radiation doses to the femur, rectum, small intestine, bladder, and bone marrow in the observation group were lower than those in the control group (all P<0.05). After treatment, serum levels of CYFRA21-1, CEA, and SCCA decreased in both groups, with the observation group showing lower levels than the control group (all P<0.05). After treatment, the percentage of CD8+ lymphocytes increased in both groups (all P<0.05), but there was no significant difference between the groups (P>0.05). The percentage of CD4+ lymphocytes and the CD4+/CD8+ ratio decreased in both groups, but the observation group had higher values than the control group (all P<0.05). The incidence of radiation enteritis in the observation group was lower than that in the control group (P<0.05). Conclusion Both IMRT and 3D-CRT are effective in treating cervical cancer, suppressing tumor markers such as CYFRA21-1, CEA, and SCCA. IMRT demonstrates stronger suppression of these markers, causes less damage to immune function, delivers lower radiation doses to organs, and offers higher safety.
【Key words】Cervical cancer; Three-dimensional conformal radiotherapy; Intensity-modulated radiotherapy; Cytokeratin 19 fragment; Carcinoembryonic antigen; Squamous cell carcinoma antigen
【Chinese Library Classification】R737.33 【Document Identification Code】 A 【Article Number】2096-2665.2024.13.0075.04
DOI: 10.3969/j.issn.2096-2665.2024.13.025
Radiotherapy is one of the primary treatment modalities for cervical cancer. Clinically, increasing the radiation dose to the tumor area is often adopted to enhance local tumor control. However, this approach also elevates the radiation exposure to surrounding normal tissues, thereby increasing the risk of related complications [1-2]. Three-dimensional conformal radiotherapy (3D-CRT) allows adjustment of radiation direction and dose distribution. Intensity-modulated radiotherapy (IMRT), developed based on 3D-CRT, enables control over the shape of the dose distribution to align with the target volume in three dimensions, thereby reducing irradiation to normal tissues [3]. While numerous studies have explored different combinations of radiotherapy regimens for cervical cancer, most focus on aspects such as radiation source selection, dosage, and treatment duration [4]. Based on this, the present study aims to evaluate the efficacy of 3D-CRT and IMRT in cervical cancer patients and analyze their impact on tumor marker levels. The findings are reported as follows.
1 Materials and Methods
1.1 General Information
A total of 82 cervical cancer patients admitted to Gansu Wuwei Cancer Hospital between June 2020 and June 2023 were enrolled in this study. They were randomly assigned to a control group and an observation group using a random number table method, with 41 cases in each group. The control group had an age range of 34–59 years and a mean age of (50.69 ± 8.14) years. Pathological types included 32 cases of squamous cell carcinoma and 9 cases of adenocarcinoma. Maximum tumor diameter was ≥4 cm in 6 cases and <4 cm in 35 cases. The observation group had an age range of 37–59 years and a mean age of (51.36 ± 7.95) years. Pathological types included 29 cases of squamous cell carcinoma and 12 cases of adenocarcinoma. Maximum tumor diameter was ≥4 cm in 9 cases and <4 cm in 32 cases. No statistically significant differences were found in the general characteristics between the two groups (all P > 0.05), indicating that the groups were comparable. This study was approved by the Medical Ethics Committee of Gansu Wuwei Cancer Hospital. All patients and their families were informed and provided written informed consent. Inclusion criteria: (1) Meeting the diagnostic criteria for cervical cancer [5]; (2) Age ≥18 years. Exclusion criteria: (1) Patients with combined hepatic or renal dysfunction; (2) Patients with metastatic tumors; (3) Patients with other malignant tumors; (4) Patients with contraindications to radiotherapy or chemotherapy.
1.2 Treatment Methods
Prior to radiotherapy, all patients underwent contrast-enhanced CT scanning with images uploaded to the Varian workstation. The scan range extended from the L2 vertebral body to the ischial tuberosity. The clinical target volume (CTV) was delineated, followed by a 0.7 cm expansion in three dimensions to outline the planning target volume (PTV). Finally, organs and tissues potentially affected during radiotherapy—including the femur, rectum, small intestine, bladder, and bone marrow—were contoured with a 2 cm margin beyond the upper and lower boundaries of the PTV. Images were transferred to the three-dimensional treatment planning system (TPS), and both groups received radiotherapy. • The control group received three-dimensional conformal radiotherapy (3D-CRT) using a four-field box technique. The dose fractionation was 2.0 Gy per session, once daily, five times per week, with a total dose of 50 Gy. • The observation group received intensity-modulated radiotherapy (IMRT) using a coplanar irradiation technique, with a four-field conformal design to optimize dose distribution. The treatment followed conventional fractionation principles to ensure uniform and clinically appropriate dose delivery. A 6MV-X ray source was used, with a single fraction dose of 2.0 Gy, administered once daily, five times per week, to maintain treatment continuity and stability. The total radiotherapy dose was set at 50 Gy to achieve the intended therapeutic effect. Optimization objectives and constraints were consistent for all patients. Some patients received additional intravaginal brachytherapy to further enhance treatment efficacy. The key reference point for brachytherapy was set at 0.5 cm below the vaginal mucosa to ensure precise dose delivery to the target area. The brachytherapy dose was 10 Gy, delivered in two fractions. Concurrent chemotherapy was administered weekly using single-agent cisplatin (Qilu Pharmaceutical Co., Ltd., National Drug Approval No. H37021356, Specification: 30 mg). Cisplatin was dosed at 40 mg/m² based on body surface area, with a maximum single dose of 150 mg. Treatment was given once every 7 days, with one cycle defined as 7 days, for a total of 5 cycles.
1.3 Observation Indicators
(1) Comparison of clinical efficacy between the two groups: Complete disappearance of lesions lasting at least 30 days was defined as complete response (CR); reduction of lesions ≥50% lasting at least 30 days was defined as partial response (PR); reduction of lesions <50% or increase of lesions <25% lasting at least 30 days was defined as stable disease (SD); increase of lesions ≥25% or appearance of new lesions was defined as progressive disease (PD) [5]. Total effective rate = CR rate + PR rate. (2) Comparison of radiation doses to different organs between the two groups: The radiation doses to the femur, rectum, small intestine, bladder, and bone marrow were measured using a medical linear accelerator (Varian Medical Systems, Inc., National Medical Device Registration No. 20163052474, Model: VitalBeam). (3) Comparison of cytokeratin 19 fragment (CYFRA21-1), carcinoembryonic antigen (CEA), squamous cell carcinoma antigen (SCCA), and T lymphocyte subset levels between the two groups: 4 mL of venous blood was collected from the elbow vein of each patient. After centrifugation for 10 minutes (speed: 3500 rpm, radius: 8 cm), serum was separated. CYFRA21-1, CEA, and SCCA levels were detected using enzyme-linked immunosorbent assay (ELISA). Another 4 mL of venous blood was drawn from the elbow vein, and the percentages of CD4 and CD8 T lymphocytes were measured using a flow cytometer (Becton, Dickinson and Company, BD Biosciences, National Medical Device Registration No. 20152403509, Model: BD FACS Calibur). The CD4+/CD8+ ratio was calculated (measured before treatment and one month after treatment). (4) Comparison of complications between the two groups: Complications included radiation enteritis, radiation cystitis, digestive system reactions, leukopenia, and thrombocytopenia.
1.4 Statistical Analysis
The data were processed using SPSS 22.0 statistical software. Count data were expressed as [n (%)] and analyzed by chi-square test or rank-sum test; measurement data were expressed as (x̄±s) and analyzed by t-test. A p-value <0.05 was considered statistically significant.
2 Results
2.1 Comparison of Clinical Efficacy Between the Two Groups
No statistically significant differences were found in overall efficacy or total effective rate between the two groups (all P>0.05), as shown in Table 1.
Table 1 Comparison of Clinical Efficacy Between the Two Groups [n (%)]
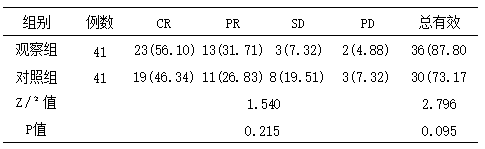
Note: CR: Complete response; PR: Partial response; SD: Stable disease; PD: Progressive disease
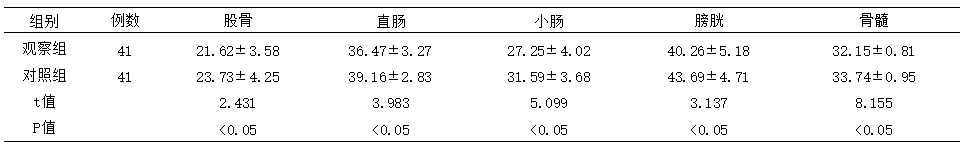
2.2 Comparison of Radiation Doses to Different Organs Between the Two Groups
The observation group showed significantly lower radiation doses to the femur, rectum, small intestine, bladder, and bone marrow compared to the control group, with statistically significant differences (all P<0.05), as detailed in Table 2.
Table 2 Comparison of Radiation Doses to Different Organs Between the Two Groups (Gy, x̅±s)
2.3 Comparison of Serum CYFRA21-1, CEA, and SCCA Levels Between the Two Groups
Before treatment, no statistically significant differences were observed in serum CYFRA21-1, CEA, or SCCA levels between the two groups (all P>0.05). After treatment, both groups showed decreased levels of these markers, with the observation group demonstrating significantly lower values compared to the control group (all P<0.05). See Table 3 for details.
Table 3 Comparison of Serum CYFRA21-1, CEA, and SCCA Levels Between the Two Groups (x̅±s)
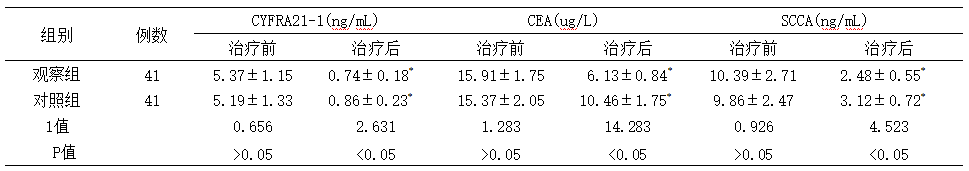
Note: Compared with pre-treatment values within the same group, *P<0.05. CYFRA21-1: Cytokeratin 19 fragment; CEA: Carcinoembryonic antigen; SCCA: Squamous cell carcinoma antigen.
2.4 Comparison of T Lymphocyte Subset Levels Between the Two Groups
Before treatment, no statistically significant differences were observed in the percentages of CD4⁺ T cells, CD8⁺ T cells, or the CD4⁺/CD8⁺ ratio between the two groups (all P>0.05). After treatment, both groups showed an increase in CD8⁺ T cell percentages with statistical significance (P<0.05), though no significant difference was found between the groups (P>0.05). Both groups exhibited decreases in CD4⁺ T cell percentages and the CD4⁺/CD8⁺ ratio; however, the observation group demonstrated significantly higher values compared to the control group (all P<0.05). See Table 4 for details.
Table 4 Comparison of T Lymphocyte Subset Levels Between the Two Groups (x̅±s)
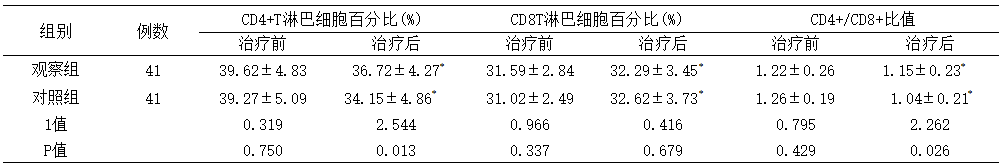
Note: Compared with pre-treatment levels within the same group,*P<0.05
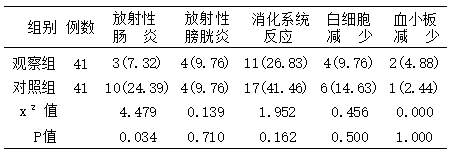
2.5 Comparison of Complications Between the Two Groups
The incidence of radiation enteritis in the observation group was significantly lower than that in the control group, with a statistically significant difference (P<0.05). No statistically significant differences were observed in the incidence of radiation cystitis, gastrointestinal reactions, leukopenia, or thrombocytopenia between the two groups (all P>0.05), as shown in Table 5.
Table 5 Comparison of Complications Between the Two Groups [n (%)]
3 Discussion
With the iterative development of technologies such as computing, radiation physics, and imaging, both research and clinical applications of cancer radiotherapy have continuously advanced. Sophisticated radiation therapy techniques including three-dimensional conformal radiotherapy (3D-CRT) and intensity-modulated radiotherapy (IMRT) have been increasingly adopted, benefiting a growing number of cervical cancer patients. This study aims to evaluate the efficacy of 3D-CRT and IMRT in cervical cancer treatment, with the expectation of providing valuable insights for clinical decision-making regarding radiotherapy modalities.
The results of this study showed no statistically significant differences in efficacy between the two groups, indicating that both three-dimensional conformal radiotherapy (3D-CRT) and intensity-modulated radiotherapy (IMRT) achieved favorable therapeutic outcomes for cervical cancer. Additionally, the observation group demonstrated significantly lower radiation doses to the femur, rectum, small intestine, bladder, and bone marrow compared to the control group, suggesting that IMRT can reduce radiation exposure to adjacent organs compared to 3D-CRT, thereby mitigating damage to critical organs. As an advanced form of three-dimensional radiotherapy evolved from 3D-CRT, IMRT enables precise targeting by integrating three-dimensional anatomical data of lesions. This technique offers superior radiation precision over 3D-CRT, further minimizing radiation-induced damage to surrounding tissues and organs [7].
CYFRA21-1 is a highly sensitive tumor marker particularly for lung cancer; CEA is a broad-spectrum tumor marker that may be highly expressed in various malignant tumors, with significantly elevated levels especially in colorectal cancer, gastric cancer, and lung cancer; SCCA is primarily expressed in squamous cell carcinoma tissues, such as lung cancer, cervical cancer, and head and neck cancer. These factors can serve as auxiliary diagnostic indicators and disease monitoring parameters for cancer. The results of this study showed that serum levels of CYFRA21-1, CEA, and SCCA in the observation group were lower than those in the control group after treatment, suggesting that both methods can suppress tumor marker levels, with intensity-modulated radiotherapy demonstrating superior efficacy. CYFRA21-1, CEA, and SCCA are expressed at low levels in healthy populations, but their serum expression increases following carcinogenesis, reflecting tumor infiltration and growth [8]. Both radiotherapy techniques inhibit tumor cell replication and induce cancer cell apoptosis through targeted radiation delivery, thereby suppressing tumor growth and reducing serum tumor marker levels. The lower levels of CYFRA21-1, CEA, and SCCA in the observation group indicate that intensity-modulated radiotherapy is more effective in inhibiting tumor cell proliferation and alleviating disease progression.
The results of this study showed that after treatment, the percentage of CD4⁺ T lymphocytes and the CD4⁺/CD8⁺ ratio decreased in both groups, but the observation group exhibited higher values than the control group. This suggests that both methods induced immunosuppression, but intensity-modulated radiotherapy (IMRT) resulted in relatively milder immunosuppression. This may be attributed to IMRT's optimized irradiation field parameters, which help control post-radiation damage repair in cells, protect organs at risk, mitigate radiation-induced injury, while maintaining better therapeutic efficacy [9]. Additionally, the incidence of radiation enteritis was lower in the observation group than in the control group, indicating fewer adverse reactions with IMRT. The underlying reason is that IMRT reduces radiation exposure to organs adjacent to the tumor, ensures adequate tumor dose coverage, minimizes damage to tissues and the immune system, thereby lowering the risk of adverse reactions in patients [10].
In summary, compared with three-dimensional conformal radiotherapy, intensity-modulated radiotherapy demonstrates superior efficacy in suppressing serum tumor markers such as CYFRA21-1, CEA, and SCCA in cervical cancer patients. It also reduces radiation exposure to adjacent organs, causes milder immunosuppressive effects, and exhibits a more favorable safety profile.
References
[1] 乔友林,赵宇倩. 宫颈癌的流行病学现状和预防 [J/CD]. 中华妇幼临床医学杂志(电子版),2015,11(2): 1-6.
[2] 沈志勇,林建海,廖绍光,等. 子宫颈癌术后调强放疗和三维适形放疗的临床疗效观察[J]. 临床肿瘤学杂志,2016,21(10): 903-908.
[3] 邓鹏,李必波,伍俞霓. 调强放疗与三维适形放疗在宫颈癌治疗中的应用比较[J]. 实用癌症杂志,2019,34(11): 1902-1904.
[4] 乔志安,杨立鑫,王晓贞. 三维适形放疗与调强放疗分别联合腔内后装放疗治疗中晚期宫颈癌的效果对比[J]. 中国医药导报,2017,14(29): 89-92.
[5] 中国抗癌协会妇科肿瘤专业委员会. 宫颈癌诊断与治疗指南(第四版)[J]. 中国实用妇科与产科杂志,2018,34(6): 613-622.
[6] 崔小妹,钱立庭,崔亚云,等. 中晚期宫颈癌适形调强放疗联合三维腔内后装放疗的剂量学初步研究[J]. 现代妇产科进展,2019,28(1): 31-34.
[7] 张明旺,张恒. 中晚期宫颈癌调强放疗与三维适形放疗的临床疗效对比研究[J]. 川北医学院学报,2023,38(9): 1227-1231.
[8] 王飞霞,杨瑞利,韩双. 细胞DNA定量分析联合HR-HPV、SCCA、CYFRA21-1检测在早期宫颈癌筛查中的价值[J]. 肿瘤杂志,2018,24(3): 281-284.
[9] 景莉,翟蓓蓓,王军良. 宫颈癌调强放疗与三维适形放疗疗效对比观察[J]. 人民军医,2021,64(8): 751-753.
[10] 蒋军,张利文,廖珊,等. 三维适形放疗、调强放疗和容积调强放疗在宫颈癌术后患者中的应用[J]. 广西医学,2020,41(18): 2426-2429.
Preliminary Review: Liu Wenyu
Final Review: Ma Shuqian
