Carbon Ion Therapy for Skull Base Chordoma
Carbon Ion Therapy for Skull Base Chordoma
Ⅰ.Overview
Skull base chordoma is a low-grade malignant bone tumor originating from ectopic or residual embryonic notochord tissue. It almost exclusively involves the axial skeleton, with 35%–40% occurring at the chondral junction of the spheno-occipital region of the skull base, while the remaining cases occur in other parts of the spine. Skull base chordomas are commonly found in the middle and upper two-thirds of the clivus, the sellar region, and the middle cranial fossa, accounting for approximately 0.1%–0.67% of intracranial tumors. Based on their location, intracranial chordomas are generally classified into four types: sellar type, clivus-posterior fossa type, middle cranial fossa type, and nasopharyngeal type.
Surgical resection is the primary treatment for skull base chordoma, with the goal of achieving complete tumor removal. Even if complete resection is not possible, surgery can reduce tumor volume and alleviate compression of critical organs such as the brainstem and optic pathways, creating conditions for subsequent radiotherapy. Due to the difficulty in achieving complete resection and the high local recurrence rate, most scholars advocate postoperative radiotherapy as a standard practice, regardless of the extent of surgical resection. For patients who are not candidates for surgery, biopsy followed by radiotherapy is a feasible treatment option, and radical radiotherapy alone can also be considered.
Based on the type of radiation, radiotherapy mainly includes conventional photon radiation, proton radiation, and heavy ion (primarily carbon ion) radiation. Due to the poor radiosensitivity of chordomas and the proximity of the skull base to critical normal tissues (such as the brainstem, optic nerves, and optic chiasm), conventional photon radiotherapy often yields suboptimal results. Proton or heavy ion radiation, however, can focus the radiation more precisely on the tumor area and has a stronger tumor-killing effect. Therefore, proton and heavy ion radiation are considered first-line radiotherapy techniques for chordoma.
Carbon ion therapy, in particular, has shown significant advantages in treating skull base chordomas. It delivers high-energy carbon ions that precisely target the tumor while minimizing damage to surrounding healthy tissues, making it an effective and safe treatment option for this challenging condition.
II. Target Delineation for Chordoma:
| The radiation target volume and its definitions | ||
|---|---|---|
| chordoma | GTV | The tumor visible on imaging, with the surgical bed delineated as GTVtb after complete resection. |
| CTV | Based on the subclinical extent of the tumor as suggested by imaging, the CTV typically extends 10–20 mm beyond the GTV. If the tumor involves the anterior cervical spine or prevertebral muscles, the high-risk area should include the entire clivus, cervical spine, and prevertebral muscles. Additionally, critical organs at risk (OARs) such as the brainstem, optic pathways, and spinal cord should be avoided with a 3 mm margin. | |
Target Volume Definition
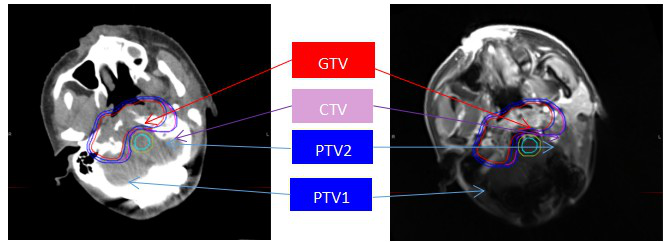
(1)Non-contrast CT (2)T1 C+
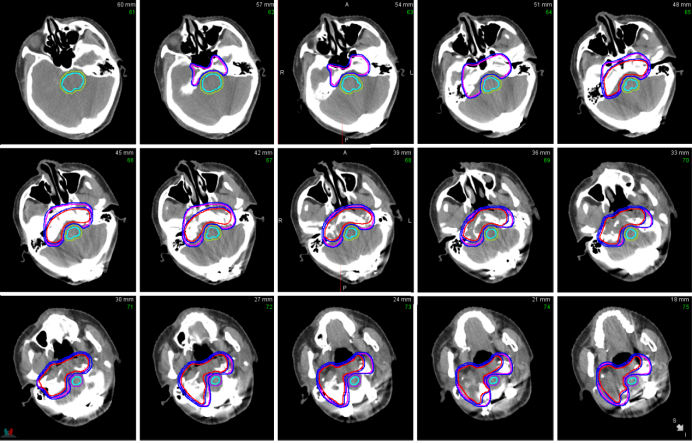
Figure 1: Illustration of target volume delineation for a case of skull base chordoma. The red area represents the GTV, the pink area represents the CTV, and the blue lines indicate PTV1 and PTV2.
III. Irradiation Techniques and Dose Fractionation
For chordoma radiotherapy, full-course carbon ion radiotherapy is a commonly used method. Based on the condition, the following prescription doses are recommended:
- For chordoma without surgery, postoperative residual, or recurrent cases:
- For chordoma suitable for complete resection:
When delineating and limiting normal organs, special attention should be paid to the dose constraints of organs at risk (OARs). The OARs that need to be delineated and limited include the brainstem, cochlea, lens, eyeballs, optic nerves, optic chiasm, hippocampus, etc. The dose constraints for OARs can be referred to in Appendix VI.
IV. Precautions
Chordoma radiotherapy requires high-dose radiation, but for tumors close to critical structures such as the brain and spinal cord, high-dose radiation can severely damage surrounding normal tissues. Therefore, chordoma radiotherapy must be highly conformal, focusing the radiation on the tumor while sparing surrounding tissues. A treatment dose below 60 Gy (RBE) is associated with poor efficacy, with most patients succumbing to local tumor progression. Thus, at least 60 Gy (RBE) of carbon ion irradiation is required. If the cervical spine has undergone metal fixation, the positioning, field direction, and radiotherapy dose should be discussed with the physicist and technician.
V. Toxicities and Side Effects
1.Acute Toxicity: Acute radiation reactions refer to temporary symptoms occurring within 6 weeks of treatment initiation. Skull base chordomas often grow in the clivus, potentially causing headaches, cranial nerve palsies, and bilateral abducens nerve palsies. During treatment, symptoms such as headaches and vision loss may worsen. The most common acute reactions include alopecia and mucositis, which generally resolve after treatment.
2.Late Toxicity: Late reactions refer to side effects occurring more than 3 months after treatment. Cranial nerve damage may lead to dysphagia, coughing while drinking, dysarthria, tongue deviation, and tongue muscle atrophy. Damage to the optic nerves and chiasm may cause vision loss, visual field changes, or even blindness. Involvement of the conduction tracts may manifest as limb weakness, hemiplegia, or loss of pain and temperature sensation. Damage to the medullary spinocerebellar tracts may result in gait abnormalities and unsteady walking. The impact of radiation damage on the brainstem varies, and some patients may experience symptom relief with early intervention. Temporal lobe and hippocampal damage can lead to impairments in brain physiological and cognitive functions, particularly affecting memory, learning, and spatial information processing.
VI. Clinical Research Progress and Prognosis
Recent studies suggest that charged particle therapy for skull base chordoma is a promising treatment method, increasing the 5-year local control (LC) rate from 69.6% to 75.8%. However, due to the slow growth of skull base chordoma, a 5-year assessment post-treatment may not be sufficiently accurate. Munzenrider et al. found that among 169 skull base chordoma patients treated with photon plus proton therapy, the 5-year and 10-year LC rates were 73% and 54%, respectively. Uhl et al. reported that among 155 skull base chordoma patients treated with carbon ion therapy, the 5-year and 10-year LC rates were 72% and 54%, respectively, with a median follow-up of 108 months (range: 9–175 months) and no loss to follow-up. Additionally, Masashi et al. conducted a retrospective analysis of 34 skull base chordoma patients treated with carbon ion radiotherapy at 60.8 Gy (RBE) / 16 fractions, 4 times per week, and found that the 5-year and 9-year LC rates improved to 76.9% and 69.2%, respectively, with local-regional control rates of 74.3% and 66.5%. During follow-up, 10 patients developed distant metastases, with estimated 5-year and 9-year distant metastasis rates of 10.1%. Although the number of patients with local recurrence was small, 8 cases had in-field recurrence, 1 had marginal recurrence, and 1 had both in-field and marginal recurrence. Among the 2 cases with local recurrence, 1 involved the skull base and 1 involved the nasal septum. Overall, carbon ion radiotherapy at 60.8 Gy (RBE) / 16 fractions is a highly promising treatment method with acceptable toxicity. Furthermore, the new spot-scanning irradiation method can further improve tumor control rates and reduce adverse reactions.
Reference
1. Amit M, Na'ara S, Binenbaum Y, Billan S, Sviri G, Cohen JT, Gil Z. Treatment and Outcome of Patients with Skull Base Chordoma: A Meta-analysis. J Neurol Surg B Skull Base. 2014 Dec;75(6):383-90.
2. Takagi M, Demizu Y, Nagano F, Terashima K, Fujii O, Jin D, Mima M, Niwa Y, Katsui K, Suga M, Yamashita T, Akagi T, Sakata KI, Fuwa N, Okimoto T. Treatment outcomes of proton or carbon ion therapy for skull base chordoma: a retrospective study. Radiat Oncol. 2018 Nov 26;13(1):232.
3. Takagi, M., Demizu, Y. Nagano, F. et al. Treatment outcomes of proton or carbon ion therapy for skull base chordoma: a retrospective study.Radiat Oncol 13, 232 (2018).
4. Jonas Johansson, Erik Blomquist, Anders Montelius, Ulf Isacsson, Bengt Glimelius,Potential outcomes of modalities and techniques in radiotherapy for patients with hypopharyngeal carcinoma,Radiotherapy and Oncology,Volume 72, Issue 2,2004,Pages 129-138.
5. Oliver Jäkel, Beate Land, Stephanie Elisabeth Combs, Daniela Schulz-Ertner, Jürgen Debus,On the cost-effectiveness of Carbon ion radiation therapy for skull base chordoma,Radiotherapy and Oncology,Volume 83, Issue 2,2007,Pages 133-138.
6. Jäkel O, Land B, Combs SE, Schulz-Ertner D, Debus J. On the cost-effectiveness of Carbon ion radiation therapy for skull base chordoma. Radiother Oncol. 2007 May;83(2):133-8.
7. Guan X, Gao J, Hu J, Hu W, Yang J, Qiu X, Hu C, Kong L, Lu JJ. The preliminary results of proton and carbon ion therapy for chordoma and chondrosarcoma of the skull base and cervical spine. Radiat Oncol. 2019 Nov 21;14(1):206.
8. Mizoe JE. Review of carbon ion radiotherapy for skull base tumors (especially chordomas). Rep Pract Oncol Radiother. 2016 Jul-Aug;21(4):356-60.
9. Lu VM, O'Connor KP, Mahajan A, Carlson ML, Van Gompel JJ. Carbon ion radiotherapy for skull base chordomas and chondrosarcomas: a systematic review and meta-analysis of local control, survival, and toxicity outcomes. J Neurooncol. 2020 May;147(3):503-513.
10. van Koevering K, Prevedello DM, Carrau RL. Endoscopic endonasal approaches for the management of cranial base malignancies: histologically guided treatment and clinical outcomes. J Neurosurg Sci. 2018 Dec;62(6):667-681.
11. Munzenrider JE, Liebsch NJ. Proton therapy for tumors of the skull base. Strahlenther Onkol. 1999;175:57-63.
12. Uhl M, Mattke M, Welzel T, et al. Highly effective treatment of skull base chordoma with carbon ion irradiation using a raster scan technique in 155 patients: first long-term results. Cancer. 2014;120:3410-3417.
13. Mizoe JE, Hasegawa A, Takagi R, Bessho H, Onda T, Tsujii H. Carbon ion radiotherapy for skull base chordoma. Skull Base. 2009;19:219-2.
