The case report ---- Pharyngeal Cancer
The case report ---- Pharyngeal Cancer.
Male patient, 57 years old, chief complaint: difficulty swallowing for six months, diagnosed with hypopharyngeal cancer half a month ago.
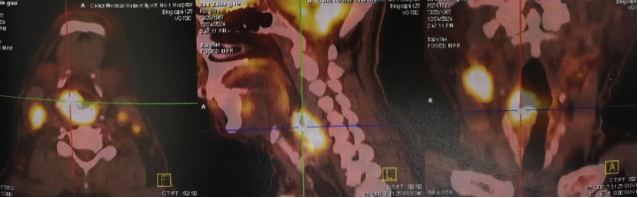
The patient experienced difficulty swallowing without apparent cause on July 1, 2024, with no symptoms of hoarseness or breathing difficulties. The symptoms worsened compared to before by December 2024. On December 24, 2024, the patient sought medical attention at the First Affiliated Hospital of China Medical University. An otolaryngology electronic laryngoscopy examination revealed an irregular new growth located on the outer wall of the right piriform fossa, retropharynx, esophageal inlet, bilateral tonsillar fossae, bilateral piriform sinuses, posterior wall of the hypopharynx, right lateral wall of the hypopharynx, and right tonsillar pillar. PET-CT showed irregular soft tissue shadows with increased metabolism (SUV of 31.7) in the right piriform fossa area and posterior region, right lateral and posterior walls of the hypopharynx, and upper end of the esophagus, suggesting a high likelihood of malignant lesions. Additionally, multiple enlarged lymph nodes were observed in the bilateral neck and supraclavicular regions, with the largest diameter measuring approximately 19mm and increased metabolism (SUV of 22.2), indicating likely metastases from malignant lesions.
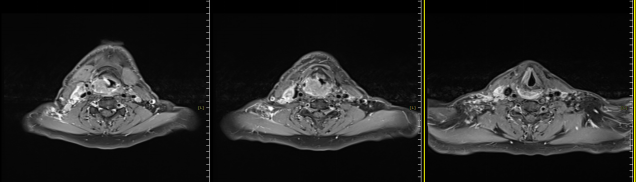
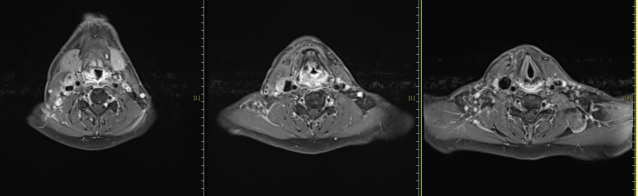
The patient was admitted to our hospital on January 7, 2025, and underwent multidisciplinary consultation before receiving carbon ion therapy for hypopharyngeal malignant tumor on January 16, 2025. The prescribed doses were as follows: PTVp: 68Gy (RBE) / 17Fx, PTVnd-L: D95% = 64Gy (RBE) / 16Fx, PTVR: 60Gy / 15Fx, PTVL: 56Gy (RBE) / 14Fx. Concurrently, cisplatin monotherapy combined with nimotuzumab injection for targeted therapy was administered. A follow-up neck MRI showed a reduction in the primary lesion and bilateral neck lymph nodes compared to pre-treatment, with a recent evaluation indicating a partial response (PR).
MRI before carbon ion therapy
MRI after carbon ion therapy
Discussion:
Hypopharyngeal cancer refers to malignant tumors originating from the epithelial tissue of the hypopharynx, also known as laryngopharyngeal cancer. It commonly occurs in the piriform sinus, accounting for approximately 51% to 59% of cases; the posterior pharyngeal wall accounts for 8% to 35%; and the retropharyngeal area accounts for 6% to 41%. In China, hypopharyngeal cancer comprises about 0.8% to 1.5% of head and neck tumors. This condition is more prevalent in males, with a male-to-female ratio of 7 to 8:1. The age of onset is most commonly between 50 and 70 years. Epidemiological studies have found that this disease is associated with excessive stimulation from tobacco and alcohol, along with certain nutritional deficiencies. Over 95% of pathological types are poorly differentiated squamous cell carcinomas, while less common types include adenocarcinomas of minor salivary gland origin, malignant lymphomas, and soft tissue sarcomas. The growth and expansion patterns are characterized by infiltration along the mucosa or submucosa. The vast majority exhibit infiltrative growth, with only a small proportion showing expansive growth.

The treatment principles for hypopharyngeal cancer focus on improving the local control rate of the tumor while minimizing damage to the functions of the laryngopharyngeal organs, aiming to preserve the normal physiological functions of the laryngopharynx and larynx as much as possible. The optimal treatment modality can be selected based on clinical staging. For early-stage hypopharyngeal cancer, the efficacy of surgical treatment is generally comparable to that of radiotherapy alone, and radiotherapy alone can help preserve the function of the laryngopharynx. Therefore, radical radiotherapy should be the first choice for stage I hypopharyngeal cancer. For stage II or III hypopharyngeal cancer, a combination of surgery followed by postoperative radiotherapy and chemotherapy can be considered. For stage IV patients without distant metastases, induction chemotherapy followed by surgery and postoperative radiotherapy and chemotherapy can be used. However, for stage IV patients with distant metastases, chemotherapy should be the primary treatment.
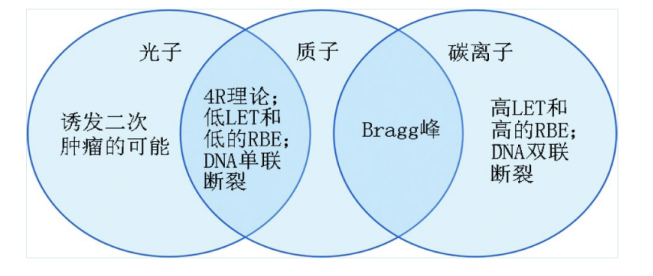
Carbon ion radio therapy (CIRT) is an emerging radiotherapy modality in the 21st century. Compared to photon radiotherapy, CIRT can improve the distribution of radiation doses, enhance the biological effects of radiation, and more effectively kill tumor cells. Since the application of carbon ion beam therapy for treating malignant tumors began in Japan in 1994, only a few countries globally, including Germany, China, Italy, and Austria, have utilized carbon ions in clinical settings. The Wuwei Heavy Ion Accelerator is the first tumor treatment device in China with independent intellectual property rights for heavy ion therapy. It can achieve two treatment modes: uniform scanning and spot scanning. It officially started clinical application in March 2020, treating malignancies such as head and neck tumors, lung cancer, liver cancer, and pancreatic cancer, accumulating rich clinical experience to date.
Recent efficacy evaluation of patients with locally advanced hypopharyngeal cancer who underwent carbon ion radiotherapy combined with concurrent chemotherapy has shown partial remission. Additionally, the patients experienced significant symptom improvement, mild side effects, and good tolerance. This confirms the effectiveness and safety of carbon ion radiotherapy in the treatment of hypopharyngeal cancer.
Radiation Oncology Department Five: Hu Tingchao, Wang Xinlan, Zhang Yaoling, Ma Shuping, Zhang Tian'e, Tong Zongze.
