Dosimetric Effect of Flattening Filter Free Mode on Liver Cancer Treatment
Dosimetric Impact of Flattening Filter-Free Mode on Volumetric Modulated Arc Therapy Plans for Liver Cancer Patients
SHI Zike, MA Xiaoyun, ZHANG Yanshan, JIN Xueling, KOU Hairui, WU Jiaming
(Department of Radiation Physics, Gansu Wuwei Tumor Hospital Heavy lon Center, Wuwei 733000,China)
[ABSTRACT] Objective To investigate the dosimetric influence of flattening filter volumetric modulated arc therapy (FF-VMAT) versus flattening filter-free volumetric modulated arc therapy (FFF-VMAT) on radiotherapy planning for patients with liver cancer using a linear accelerator with 6 MV X-ray. Methods A total of 10 patients who were diagnosed with liver cancer in Wuwei Tumor Hospital of Gansu Province from August 2020 to April 2021 and planned to undergo radiotherapy were enrolled, and 6 MV X-ray was used to design FF-VMAT and FFF-VMAT plans. The two treatment plans were compared in terms of conformity index (CI) and homogeneity index (HI) of target volume, dose distribution in normal liver tissue and organ at risk (OAR), and monitor units and beam-on time of the accelerator. Results The target dosimetric distribution of both FF-VMAT and FFF-VMAT plans can meet the clinical requirements for prescribed dose. There was a significant difference in the beam-on time of the accelerator between the two plans (t=13.611,P<0.001), while there were no significant differences between the two plans in CI and HI of target volume, dose distribution in normal liver tissue and OAR, and number of monitor units (P>0.05). Conclusion Both FF-VMAT and FFF-VMAT plans can meet the needs of clinical treatment, but FFF-VMAT plan has a shorter beam-on time and a higher treatment efficiency, and therefore, FFF-VMAT plan has more advantages when applied in clinical radiotherapy for liver cancer.
[KEY WORDS] Liver neoplasms; Radiotherapy, computer assisted; Volumetric modulated are therapy; Flattening filter free; Organ endangering dose; Dose-response relationship, radiation; Particle accelerators
[Chinese Library Classification] R735.7; R815 [Document Code] A
Liver cancer is one of the common malignant tumors in China, ranking 4th in incidence and 2nd in mortality among all malignant tumors. Approximately 260,000 new cases are diagnosed worldwide annually, with China accounting for 42% to 45% of these cases [1-2]. Radiotherapy techniques are increasingly being used in the treatment of liver cancer [3]. Volumetric modulated arc therapy (VMAT) utilizes dynamic multi-leaf collimators (MLC), variable dose rates, and variable gantry rotation speeds [4-5] to deliver rotational treatment through optimized arc irradiation, theoretically achieving better target dose distribution and reducing dose to normal tissues [6-7]. The flattening filter-free (FFF) mode removes the flattening filter, reducing head scatter factors and collimator scatter factors, resulting in smaller off-axis dose ratios and lower dose around the radiation field, thereby increasing the dose rate. The dose distribution of its radiation field significantly differs from that under the flattening filter (FF) mode [8-10]. This study developed two VMAT plans for liver cancer patients under FFF and FF modes, respectively, to compare and analyze the dosimetric differences in the target area and organs at risk (OARs), and to explore the advantages of FFF-VMAT plans for clinical radiotherapy of liver cancer.
1 Objects and Methods
1.1 Objects
A total of 10 patients diagnosed with liver cancer and receiving radiotherapy at the Heavy Ion Center of Gansu Wuwei Cancer Hospital from August 2020 to April 2021 were selected, with target volumes ranging from 35 to 200 cm³ and ages between 52 and 81 years.
1.2 Devices
VitalBeam linear accelerator (Varian Medical Systems, USA), Definition AS 64-slice large-bore CT simulator (Siemens, Germany), vacuum bag and thermoplastic membrane immobilization devices.
1.3 Methods
1.3.1 Target Volume Delineation and Prescription Dose
Patients underwent contrast-enhanced CT scans with a range from the 5th thoracic vertebra to the 4th lumbar vertebra and a slice thickness of 3 mm. The acquired CT images were transmitted in DICOM format to the treatment planning system for three-dimensional reconstruction. Radiation oncologists at our center delineated the planning target volume (PTV) and organs at risk (OARs). The prescribed dose for the target area was 50 Gy in 25 fractions [1,5]. Dose constraints for OARs were set as follows: stomach Dmax≤4500 cGy, bilateral kidneys Dmean≤1500 cGy, duodenum Dmax≤5000 cGy, spinal cord Dmax≤4500 cGy, bilateral lungs Dmean≤1500 cGy, and liver Dmean≤2500 cGy。
1.3.2 Design of Two Treatment Plans
The Eclipse 15.5 treatment planning system was used to develop two separate VMAT treatment plans for each patient: one in FFF mode and one in FF mode. The FFF mode plan utilized 6MV-FFF energy with a maximum dose rate of 1400 MU/min, while the FF mode plan utilized 6MV energy with a maximum dose rate of 600 MU/min [11]. Both treatment plans employed VMAT technology. To achieve better dose homogeneity in the target area and better protect normal liver tissue, all plans were designed with three small partial arcs (collimator angles of 5° to 20°) [12-13]. To minimize comparative bias, both plans used identical beam angles and optimization conditions. The normalization method ensured that 95% of the PTV received the prescribed dose, and the volume enclosed by 110% of the prescribed dose did not exceed 1% of the target volume.
1.3.3 Evaluation Indicators and Their Criteria for Two Treatment Plans
A comparative analysis of dose distribution cloud maps was conducted for both FFF and FF mode treatment plans. Evaluation metrics included target conformity index (CI) and homogeneity index (HI) (a CI value closer to 1 indicates better target conformity; an HI value closer to 0 indicates better dose homogeneity) [14-15], as well as dose to normal liver tissue and OARs, total monitor units (MU), and beam-on time. Specifically, CI=(PTV₉₅/VPTV)×(PTV₉₅/V₉₅),where PTV₉₅ is the volume of PTV covered by the 95% prescription isodose line, VPTV is the volume of the PTV, and V₉₅ is the total volume enclosed by the 95% prescription isodose line. HI = (D₂% — D₉₈%) / D₅%. OAR dose evaluation metrics included Dmean, Dmax, V₅, V₁₀, V₁₅, V₂₀, V₂₅, V₃₀, V₃₅, and V₄₀. The total MU and beam-on time for both radiotherapy plans were recorded.
1.4 Statistical processing
Data analysis was performed using SPSS 26.0. Measurement data were expressed as mean ± standard deviation (x̄ ± s) or median (P25, P75) (data for the right kidney and duodenum did not follow a normal distribution and were described using median values). Statistical comparisons were conducted using paired t-tests or non-parametric rank-sum tests. A p-value < 0.05 was considered statistically significant.
2 Results
2.1 Comparison of dose distribution cloud maps between the two treatment plans
Both FF-VMAT and FFF-VMAT plans met the clinical prescription requirements. Dose distribution cloud maps (including axial, coronal, and sagittal views) showed that the prescription doses of both FF-VMAT and FFF-VMAT plans adequately covered the target volume with similar dose distributions. No dose hotspots were observed outside the target, and no cold spots were found within the target. Additionally, no regions exceeding 110% of the prescription dose were detected (Figure 1).
2.2 Comparison of target dose distributions between the two treatment plans
The comparison of conformity index (CI) and homogeneity index (HI) for the target volume between the two treatment plans showed no statistically significant difference (P > 0.05). The dose distributions of both plans met the requirements of the clinical prescription dose. See Table 1 and Table 2 for details.
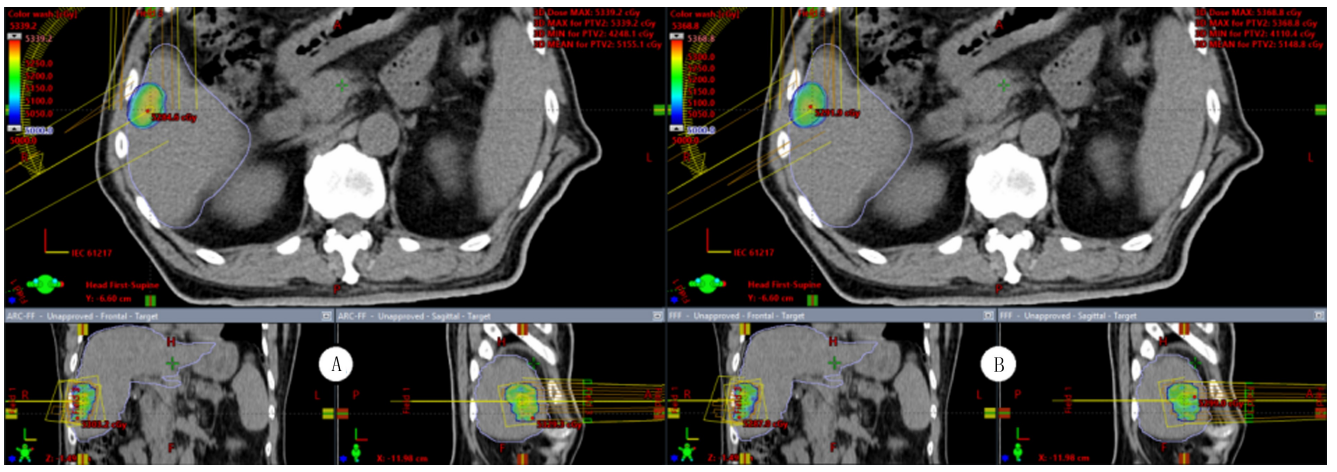
A: FF-VMAT plan,B: FFF-VMAT plan
Figure 1. Example of dose distribution cloud maps for the two treatment plans
Table 1. Comparison of CI between the two treatment plans (n=10, x̄ ± s)
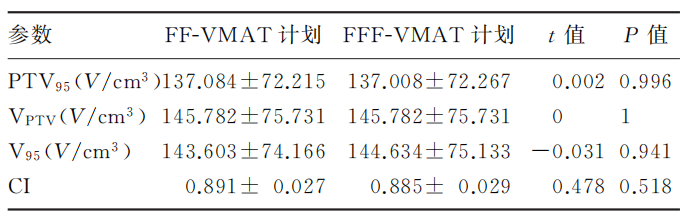
Table 2. Comparison of HI between the two treatment plans (n=10, x̄ ± s)
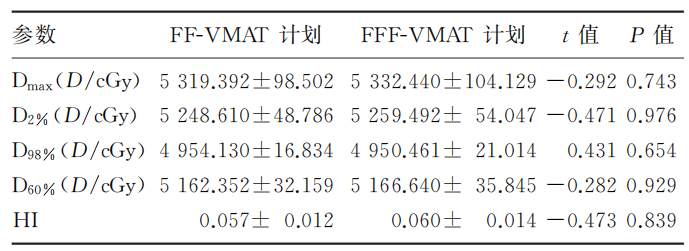
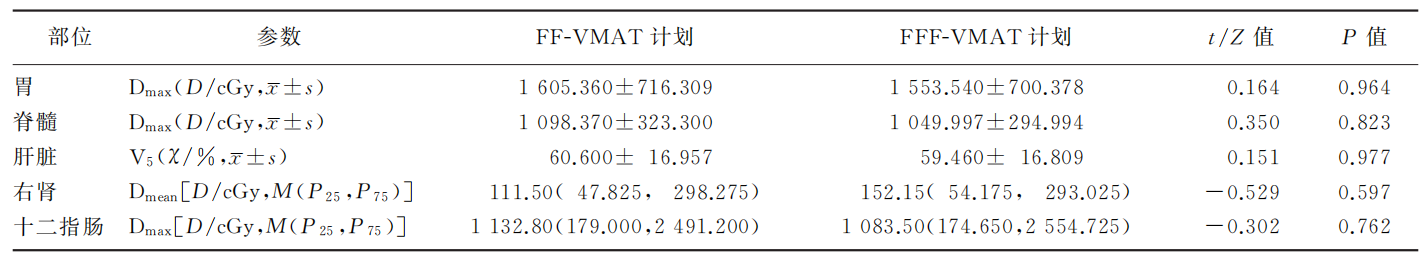
2.3 Comparison of dose distribution to normal liver tissue and OARs between the two treatment plans
Comparison of all dose parameters for normal liver tissue and OARs between the two treatment plans showed no statistically significant differences (P > 0.05), as shown in Table 3 and Table 4. The dose levels to normal liver tissue and OARs under both modes met the required dose constraints.
Table 3. Comparison of dose to normal liver tissue between the two treatment plans (n=10, x̄ ± s)
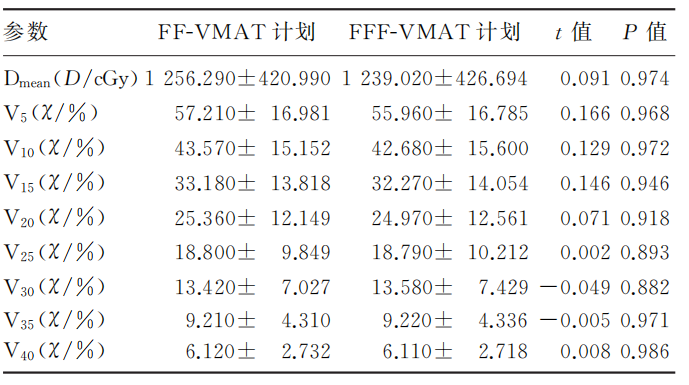
Table 4. Comparison of OAR doses between the two treatment plans (n=10, x̄ ± s)
2.4 Comparison of total monitor units and beam-on time between the two treatment plans
The total monitor units for the FF-VMAT and FFF-VMAT plans were (348.630 ± 41.747) MU and (379.800 ± 48.007) MU, respectively. The beam-on times were (0.592 ± 0.066) min and (0.271 ± 0.034) min, respectively. Comparison of the total monitor units between the two plans showed no statistically significant difference (P > 0.05). However, the comparison of beam-on time showed a statistically significant difference (t = 13.611, P < 0.05).
3 Discussion
The VMAT technique used in this study is a relatively new radiotherapy technology, with its greatest advantage being a significant improvement in treatment efficiency [4]. In recent years, the combination of VMAT technology with FFF mode has been increasingly adopted in clinical radiotherapy due to its conformal and efficient characteristics, which can enhance the therapeutic ratio for tumors. The evolution from FF to FFF mode reflects a shift in understanding among radiation oncologists and medical physicists regarding the causal relationship between the initial beam dose uniformity and the ideal final dose distribution within the target volume. The FF mode achieves beam flatness at the cost of reduced photon flux, i.e., by lowering the dose rate of the beam. In contrast, the FFF mode removes the flattening filter, resulting in a softened beam quality, lower average energy, increased photon fluence, higher dose rate, reduced beam uniformity, and smaller penumbra. This enables small-field targets to more easily achieve higher surface doses, while large-field targets may produce comparable or lower surface doses. Nevertheless, when combined with dynamic MLC modulation, the target volume can still achieve favorable conformity index (CI) and homogeneity index (HI).
The results of this study indicate that both FF-VMAT and FFF-VMAT plans met the clinical prescription dose requirements, with no significant differences observed in target conformity index (CI) and homogeneity index (HI). Zhang Jiyong et al. [16] demonstrated in a dosimetric study of rectal cancer radiotherapy that the FF mode achieved superior target dose distribution and homogeneity compared to the FFF mode, while the FFF mode was more beneficial for protecting peri-field tissues. Reggiori et al. [17] reported in a study on liver cancer that for target volumes between 100–300 cm³, the FFF mode yielded higher CI values than the FF mode, whereas for targets smaller than 100 cm³ or larger than 300 cm³, the FF mode resulted in higher CI. In contrast, Wu Sihua et al. [18] found that target volume did not significantly affect CI or HI under either mode.
The results of this study indicate that the dose fall-off outside the target volume was faster in FFF mode, with most normal liver tissues and OARs receiving lower doses. Dose distribution outside the target volume is influenced by tumor shape, size, location, degree of dose modulation, beam energy, and beam off-axis ratio [19]. Tissues outside the radiation field experience an increased off-axis ratio, and the average beam energy in FFF mode is lower than in FF mode, resulting in a more rapid dose fall-off. Related studies have also demonstrated that FFF mode can effectively protect normal tissues and OARs outside the target volume [20-22].
In this study, the irradiated volumes of normal liver tissue at 3000 cGy and 3500 cGy were slightly higher in FFF mode compared to FF mode, and the mean dose to the right kidney was also marginally elevated. This may be attributed to the greater heterogeneity of the beam quality in FFF mode, where the average energy at off-axis distances is lower than in FF mode, leading to increased scattering. Additionally, the liver cancer lesions in this study were located in the right upper abdomen with a large water-equivalent depth, which likely resulted in greater scattered dose deposition in the normal liver tissue and adjacent right kidney, thereby contributing to their slightly higher low-dose exposure [22].
In this study, the dose rate in FFF mode was 2.33 times higher than that in conventional FF mode, and the beam-on time was only half of that in FF mode. Fu et al. [23] demonstrated that the difference in treatment time between FFF and FF modes is related to the fraction dose. The larger the fraction dose, the greater the reduction in treatment time achieved with FFF mode. In radiotherapy techniques with high single-fraction doses, such as stereotactic radiosurgery (SRS) for brain tumors, stereotactic body radiotherapy (SBRT) for lung cancer, and stereotactic ablative radiotherapy (SABR) for prostate cancer, the time efficiency advantage of FFF mode can be fully utilized [18]. Due to the high single-fraction dose, the high dose rate in FFF mode effectively shortens beam-on time, thereby reducing the impact of organ motion and improving patient comfort. However, Zhou Peng et al. [24] suggested that while the high dose rate in FFF mode improves treatment efficiency, it also introduces potential risks. Therefore, techniques such as respiratory gating, image guidance, and optical surface positioning should be employed to ensure precise target localization before using FFF mode for treatment.
In summary, for radiotherapy in liver cancer patients, both FF-VMAT and FFF-VMAT modalities can meet clinical treatment requirements with no significant differences in target conformity index (CI) and homogeneity index (HI). However, the FFF-VMAT mode demonstrates faster dose fall-off outside the target volume, resulting in lower doses to normal liver tissue and organs at risk (OARs). Additionally, as this study employed conventional fractionation, the advantages of FFF-VMAT mode were not fully utilized.
【参考文献】
[1] 王维虎,曾昭冲.中国原发性肝细胞癌放射治疗指南(2020年版)[J].临床肝胆病杂志,2021,37(5):1029-1033.
[2] TSAI Y C,TSAI C L,HSU F M, et al. Superior liver sparing by combined coplanar/noncoplanar volumetric-modulated arc therapy for hepatocellular carcinoma: A planning and feasibility study[J].Med Dosim,2013,38(4):366-371.
[3] 曾昭冲.原发性肝癌放射治疗的争论与共识[J].临床肿瘤学杂志,2008,13(2):97-104.
[4] 张黎,习勉,孙文钊,等.肝癌三维适形、静态调强与容积旋转调强放射治疗的剂量学研究[J].中山大学学报(医学科学版),2012,33(3):402-406.
[5] 周冲,任洪荣,卜祥兆,等.胸上段食管癌无均整器容积弧形调强与固定野调强放疗计划的剂量学比较[J].中华放射医学与防护杂志,2015,35(4):261-264.
[6] LAI Y Q,CHEN S Y,XU C D, et al. Dosimetric superiority of flattening filter free beams for single-fraction stereotactic radiosurgery in single brain metastasis[J].Oncotarget,2017,8(21):85272-85279.
[7] RIEBER J,TONNDORF-MARTINI E,SCHRAMM O, et al. Radiosurgery with flattening-filter-free techniques in the treatment of brain metastases: Plan comparison and early clinical evaluation[J]. Strahlentherapie Und Onkologie, 2016, 192(11):789-796.
[8]贾飞,岳海振,李国文,等.有无均整器模式下鼻咽癌容积旋转调强放疗计划的剂量学比较[J].中华放射医学与防护杂志,2014,34(8):597-600.
[9]TAMILARASU S,SAMINATHAN M,SHARMA S K, et al. Comparative evaluation of a 6MV flattened beam and a flattening filter free beam for carcinoma of cervix-IMRT planning study[J].Asian Pac J Cancer Prev,2018,19(3):639-643.
[10]夏文龙,陈波,黄鹏,等.基于计划质量度量(PQM)量化比较有无均整器模式下肝癌容积旋转调强放疗计划[J].中华放射医学与防护杂志,2018,38(9):680-683.
[11]杨鑫,孙文钊,陈利,等.新型双能医用直线加速器非均整剂量学特性研究[J].中华放射肿瘤学杂志,2017,26(2):203-209.
[12]DANG T M,PETERS M J,HICKEY B, et al. Efficacy of flattening-filter-free beam in stereotactic body radiation therapy planning and treatment: A systematic review with meta-analysis[J].J Med Imaging Radiat Oncol,2017,61(3):379-387.
[13]VIEILLEVIGNE L,BESSIERES S,OUALI M, et al. Dosimetric comparison of flattened and unflattened beams for stereotactic body radiation therapy: Impact of the size of the PTV on dynamic conformal arc and volumetric modulated arc therapy[J].Phys Med,2016,32(11):1405-1414.
[14]贺先桃,谭军文,龙雨松,等.鼻咽癌FFF与FF模式下VMAT计划剂量学比较[J].中华放射肿瘤学杂志,2018,27(4):401-405.
[15]GHEMIS D M,MARCU L G. Progress and prospects of flattening filter free beam technology in radiosurgery and stereotactic body radiotherapy[J].Crit Rev Oncol Hematol,2021,163:103396.
[16]张基永,陆佳扬,吴丽丽,等.直肠癌有无均整器模式下容积旋转调强放疗的剂量学比较[J].肿瘤研究与临床,2015,27(11):732-735.
[17]REGGIORI G,MANCOSU P,CASTIGLIONI S, et al. Can volumetric modulated arc therapy with flattening filter free beams play a role in stereotactic body radiotherapy for liver lesions? A volume-based analysis[J].Med Phys,2012,39(2):1112-1118.
[18]吴思华,莫少玲,邓莹,等.非小细胞肺癌有无均整器模式下容积旋转调强放疗计划的剂量学比较[J].广东医学,2021,42(2):138-143.
[19]庄婷婷,林柏翰,李东升,等.有无均整器模式下脊柱转移瘤立体定向放疗计划的剂量学比较[J].中华放射医学与防护杂志,2016,36(1):63-66.
[20]罗红樱,周剑良,单国平,等.左侧乳腺癌术后放疗无均整器模式剂量学优势分析[J].中国医学物理学杂志,2021,38(3):281-286.
[21]牛锐,赵维秋,陈忠,等.有无均整器模式下早期乳腺癌保乳术后瘤床同期加量SWIMRT计划的剂量学研究[J].临床研究,2019,27(11):121-122.
[22]吴丽丽,张基永,陆佳扬,等.左侧乳腺癌保乳术后调强放疗有无均整器模式剂量学研究[J].第三军医大学学报,2015,37(20):2098-2101.
[23]FU W H,DAI J R,HU Y M, et al. Delivery time comparison for intensity-modulated radiation therapy with/without flattening filter:A planning study[J].Phys Med Biol,2004,49(8):1535-1547.
[24]周鹏,胡南,刘岩海,等.医用直线加速器无均整器下6MV X线能谱特性的蒙特卡罗研究[J].中国医学物理学杂志,2016,33(8):761-765.
Preliminary Review: Liu Wenyu
Final Review: Ma Shuqian
