Treatment of female urethral melanoma with carbon ion:A case report
Treatment of female urethral melanoma with carbon ion:A case report
WANG Jianhua,GUAN Zhaoyu,ZHAOZhiping,Ll Xiaobo,LI Xiaojun,ZHANG Hong
Department of Radiology,Gansu Wuwei Tumour Hospital,Gansu Wuuei 733000,China.
【Keywords】melanoma,imaging,carbon ion
Modern Oncology 2021,29(14):2535-2538
Urethral meatus melanoma is clinically rare. Most patients undergo surgical treatment after diagnosis, but the survival rate is low and metastasis is common. Heavy ion therapy for urethral meatus melanoma has been rarely reported both domestically and internationally. This case report of a female patient with urethral meatus melanoma treated with heavy ion therapy aims to enhance understanding of this disease and accumulate experience for future clinical practice.
Case Report
Patient: Female, 71 years old.
Chief Complaint:
Vaginal orifice heaviness and discomfort for 4 months, discovery of a vaginal orifice mass for 2 months.
Present Illness: As reported by the family, the patient began experiencing vaginal orifice heaviness and discomfort during strenuous physical labor in August 2018, accompanied by urinary frequency and urgency, but did not pay sufficient attention. In October 2018, the aforementioned symptoms worsened, and she incidentally noticed a "date-sized" mass at the vaginal orifice. The mass was brown, hard, non-tender, and progressively enlarged, accompanied by difficulty urinating and a burning sensation during urination.
Auxiliary Examinations:
- CT Scan (Plain): A mixed slightly hyperdense nodule at the vaginal orifice (Figure 1), with an axial size of approximately 2.1 cm × 1.8 cm. Enhanced scanning showed significant enhancement (Figure 2).
- MRI Scan (Plain): A round short-T1 slightly long-T2 nodule at the vaginal orifice, with DWI showing high signal (Figures 3–5). The ADC value was 0.88 × 10⁻³ mm²/s, and enhanced scanning showed significant enhancement (Figure 6). The urethral wall above the lesion was slightly thickened. No significantly enlarged lymph nodes were found in the pelvic cavity.
- PET/CT: An area of abnormal FDG uptake with an SUVmax of 48.6 (Figure 7).
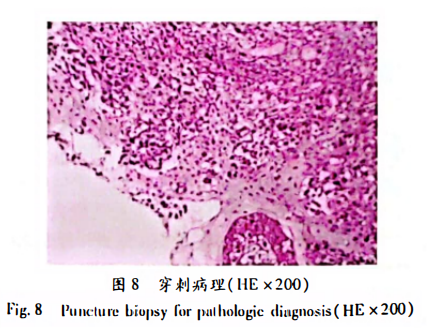
A subsequent puncture biopsy revealed: (Vaginal orifice)Based on HE morphology (Figure 8) and immunohistochemistry, the findings were consistent with malignant melanoma. Immunohistochemical markers: Tumor cells showed CKP (-), HMB45 (-), S-100 (-), Melan-A (+), Vimentin (+), CD30 (-), Ki-67 (+70%).
Specialized Examination: In the lithotomy position, at the 6 o’clock position of the vaginal orifice, between the vagina and the urethral orifice, there was a round mass. The lesion invaded the upper vaginal wall and the lower urethral wall, measuring approximately 2.5 cm × 2.0 cm × 2.0 cm. It was black, hard, with small mobility, firm texture, non-tender on palpation, without obvious ulceration or bleeding. The external urethral orifice was visible, with no purulent discharge. Scattered subcutaneous pigmentation was observed around the vaginal orifice, measuring approximately 0.5 cm × 0.3 cm (Figure 9).
Clinical Diagnosis: Vaginal orifice malignant melanoma, T4aN0M0, Stage IIb (AJCC 8th Edition). ECOG score: 1.
After multidisciplinary consultation, surgical treatment was planned. However, due to the extensive surgical damage, the patient’s family refused surgery, chemotherapy, molecular targeted therapy, and conventional radiotherapy. Therefore, the patient underwent carbon ion therapy at our hospital.
The lesion was treated with carbon ion radiotherapy, with the PTV receiving a single dose of DT 3.8 Gy(RBE)/fraction and a total dose of DT 60.8 Gy(RBE)/16 fractions. Six months after the completion of radiotherapy, follow-up imaging showed significant shrinkage of the lesion (Figure 10). The patient was followed up for 6 months with no evidence of distant metastasis. Carbon ion therapy has shown remarkable efficacy in treating melanoma, although current reports are limited. More experience needs to be accumulated.
2. Discussion
Vaginal orifice melanoma is clinically rare, accounting for only 0.2% of all melanomas and 1%–4% of urological tumors [1]. Most melanomas are located in sun-exposed areas of the skin, such as the head, neck, cheeks, trunk, and limbs, while occurrences in the vagina, nasal cavity, oral mucosa, and anus are uncommon.
Primary vaginal orifice melanoma is even rarer. Early diagnosis and treatment are crucial for patients, particularly in distinguishing between benign and malignant tumors and non-neoplastic inflammatory lesions. Melanoma originates from melanocytes derived from neural crest cells. Most melanomas occur in friction-prone areas of the skin [2], exhibiting colors ranging from black to blue or brown. When melanoma grows horizontally, it tends not to spread; however, when it grows vertically, dissemination occurs.
The incidence of vaginal orifice melanoma is low in males, often occurring in the fossa navicularis or anterior/posterior urethral orifices. The prevalence in females is three times that in males, with an average age of onset of 64 years. Studies suggest that telomeres and homologous or heterologous cellular interactions among smooth muscle cells, nerves, immune stem cells, melanocytes, red blood cells, and Schwann cells indicate their involvement in tissue structure formation and promotion of muscle contraction and immune responses. The Q94E mutation, which leads to loss of stability and dynamics in the POT1 protein, may be associated with familial melanoma [5].
This disease is prone to misdiagnosis. While the color of the lesion can aid in diagnosis, some cases show no pigmentation changes.
Clinical Manifestations:
The typical presentation includes nodules or masses at the vaginal orifice, appearing black, blue, or brown. Some patients may lack obvious pigmentation. The mass may be soft in texture, with possible surface erosion or ulceration. Some cases are accompanied by vaginal bleeding and difficulty urinating [6].
Imaging Findings:
- CT: Shows regular or irregular soft tissue nodules with homogeneous or heterogeneous density. Most lesions exhibit mild enhancement after contrast administration.
- MRI: Imaging features vary depending on the amount of melanin within the lesion. The classic MRI appearance is high signal intensity on T1-weighted images (T1W1), low signal on T2-weighted images (T2W2), and isointense to hyperintense signals on diffusion-weighted imaging (DWI), with indistinct tumor margins. When the lesion contains non-melanin components, it appears isointense or hypointense on T1W1, and isointense to hyperintense on T2W1 and DWI. A third mixed-type shows heterogeneous signals. In cases of hemorrhage within the lesion, varying stages of hemorrhagic signals may be present [7], making diagnosis more challenging. Significant enhancement is often seen on T1-weighted post-contrast imaging [8].
Definitive diagnosis requires histopathological examination. PET/CT typically shows ¹⁸F-FDG uptake, though some patients may not demonstrate uptake. PET/CT is useful for evaluating multi-organ or multi-tissue involvement, thereby improving the detection rate of early metastases. It is also recommended for the assessment of early-stage and preoperative stage III and IV melanoma lesions, as well as for evaluating early treatment response.
This condition must be differentiated from urethral caruncles, which are more common in postmenopausal women, are soft in texture, and appear as pink or red polypoid nodules [9]. They are less prone to bleeding, and histological examination can differentiate them.
Treatment:
Vaginal orifice melanoma is resistant to chemotherapy, resulting in a relatively high global mortality rate. When the lesion is localized without surrounding invasion, surgical excision may be performed. If local invasion is present or the patient is unable to tolerate surgery, radiotherapy is recommended.
In recent years, carbon ion radiotherapy has played an increasingly important role in cancer treatment. Heavy ion beam radiotherapy is an emerging radiation technology characterized by:
- Precise Dose Distribution: Enables maximal tumor destruction while minimizing damage to surrounding normal tissues.
- Ideal Biological Effect: Carbon ion beams can induce lethal damage to multiple sites on DNA double strands, effectively eradicating cancer cells.
- Dynamic Beam Monitoring: Since carbon (C) emits positron beams, positron emission tomography (PET) can monitor the distribution of carbon ions within the patient’s body. Thus, performing PET scans during or shortly after treatment allows precise control of the ion beam within the target area—an advantage unique to this modality [10].
If the mass is confined to the vaginal orifice with negative margins, surgical resection is advised. In cases with signs of local infiltration, extended surgical approaches—such as radical cystectomy—may be recommended. Radiotherapy is suitable for primary lesions in patients who are intolerant to surgery or have positive surgical margins but are not candidates for a second operation [11].
Primary melanoma is highly malignant with a poor prognosis. Late-stage patients have approximately a 25% one-year survival rate, with a median survival of less than 6 months [12].
This Case:
The patient was of advanced age, with comprehensive imaging data and a clear diagnosis. The lesion was extensive, and surgical intervention would have significantly impacted her postoperative quality of life. After receiving carbon ion radiotherapy, follow-up at 6 months showed a reduction in the primary lesion and significant relief of symptoms, with no evidence of distant metastasis. This indicates that carbon ion radiotherapy has a notable therapeutic effect on melanoma, potentially improving the patient’s progression-free survival. These findings will provide valuable guidance for both imaging and clinical professionals in diagnosis and treatment decision-making.
Preliminary Review: Zhang Jie, Final Review:Ma Shuqian
