A clinical case report on the abscopal effect of carbon ion radiotherapy
A clinical case report on the abscopal effect of carbon ion radiotherapy
中华放射医学与防护杂志 2024年8月第44卷第8期 Chin J Radiol Med Prot, August 2024, Vol. 44, No. 8
Qin Tianyan, Zhang Yihe, Zhang Yanshan, Ye Yancheng, Pan Xin, Wang Xin, Yang Yuling, Ma Tong, Lyu Caixia, Li Pengqing
Department of Radiotherapy, Wuwei Cancer Hospital of Gansu Province, Wuwei 733000, China
Corresponding author: Zhang Yihe, Email: sipen@163.com
Fund program: Scientific and Technological Projects in Gansu Province (23JRRH006)
Radiation therapy is one of the primary methods for local cancer treatment. Relevant studies have found that radiation can induce a unique immunostimulatory effect known as the abscopal effect (AE), which refers to the shrinkage of lesions outside the irradiated target area when a localized tumor lesion is treated. Carbon ion radiotherapy (CIRT) is currently the preferred method in clinical radiation therapy, offering more advantages compared to conventional radiotherapy and is believed to have the potential to activate stronger immunogenicity in tumor cells [1].
From a physical perspective, carbon ions exhibit a characteristic energy distribution in depth called the "Bragg peak," where high levels of energy are deposited in tissues near the target, while proximal tissues receive minimal energy. From a biological standpoint, carbon ions have a higher linear energy transfer (LET) and a greater relative biological effectiveness (RBE) than photons, amplifying the biological effects by at least 2–4 times in the peak region [2–4]. Due to these physical and biological advantages, CIRT is considered more capable of inducing a stronger immune response than conventional radiotherapy [5].
Research also suggests that the mechanism of the abscopal effect is attributed to a series of changes in the human immune system triggered by localized radiation therapy [6]. However, there are limited clinical and mechanistic studies on the abscopal effect induced by CIRT. Most experimental results indicate that carbon ion radiotherapy can provoke a robust pro-immunogenic response, leading to a more pronounced abscopal effect [5]. This study summarizes three typical cases of the abscopal effect observed since the Wuwei carbon ion therapy system was officially implemented for clinical treatment, providing a reference for clinical research on the abscopal effect induced by CIRT.
Ⅰ.Case Reports
Case 1:A 48-year-old female presented with the chief complaint of "palpitations and shortness of breath for 1 year, 10 years after malignant thymoma surgery." On February 16, 2009, the patient underwent "extensive thymic tumor resection + partial resection of the left upper lung lobe, phrenic nerve, and pericardium." Postoperative pathology revealed (anterior superior mediastinum) non-keratinizing squamous cell carcinoma of the thymus. Thirty-five days after surgery, the patient received postoperative intensity-modulated radiation therapy (IMRT) with a total dose of 50 Gy in 25 fractions, targeting the original tumor bed and upper mediastinum. Subsequently, the patient received no further treatment and underwent regular chest CT follow-ups.
In December 2019, the patient again experienced palpitations and shortness of breath. A repeat chest CT showed multiple nodules in the left pleura, diaphragmatic crura, and peritoneum, with the largest lesion (6.3 cm × 5.2 cm) located near the pericardium in the left pleura. Additionally, multiple small lymph nodes were observed in the left cervical root, mediastinum, and retroperitoneum, suggesting recurrent metastatic thymic carcinoma. The clinical diagnosis was recurrent metastatic thymic carcinoma, classified as T3N0M1a stage IVA according to the 8th edition of the American Joint Committee on Cancer (AJCC) staging system.
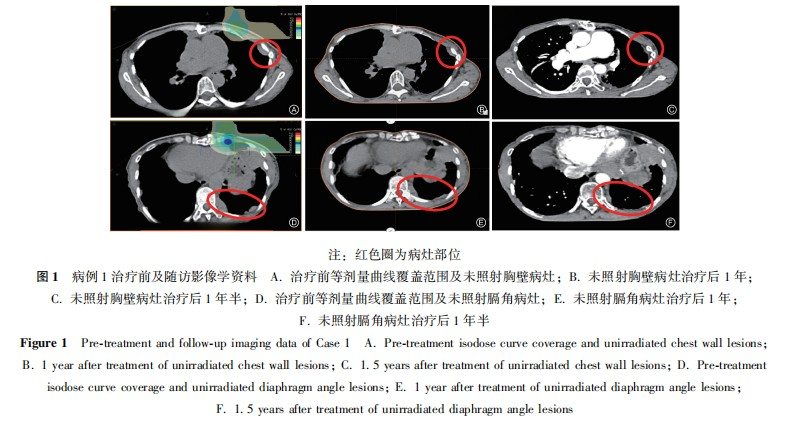
After multidisciplinary team (MDT) consultation, considering the patient's prolonged disease-free survival following the previous surgery and radiotherapy and the tumor's indolent biological behavior, palliative carbon ion radiotherapy was administered to the largest tumor near the left pericardium to alleviate cardiac compression symptoms. The treatment plan involved carbon ion therapy for the left cardiac margin lesion, with a planned target volume (PTV) dose of 60 Gy (RBE) in 12 fractions, ensuring that 90% of the PTV received the prescribed dose.
During treatment, the patient developed only mild skin pigmentation at the treatment site, diagnosed as grade 1 radiation dermatitis according to the Common Terminology Criteria for Adverse Events (CTCAE v5.0). The skin reaction resolved almost completely two months after treatment. A chest CT performed immediately after treatment completion showed shrinkage not only of the irradiated lesion (left pericardium) but also of metastatic lesions in other areas (left chest wall and left diaphragmatic crus) that had received low or no radiation. This shrinkage persisted during follow-up over the next year.
The maximum diameters of the left pericardial lesion before treatment, at treatment completion, and one year post-treatment were 6.3 cm, 4.6 cm, and 3.9 cm, respectively. The left chest wall lesion measured 2.8 cm, 1.9 cm, and 0.8 cm, while the left diaphragmatic crus lesion measured 4.1 cm, 3.9 cm, and 3.4 cm at these time points. According to Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1:
• Complete response (CR):Disappearance of all target lesions, with lymph node short-axis diameter <10 mm, sustained for at least 4 weeks.
• Partial response (PR): ≥30% reduction in the sum of the longest diameters of target lesions, sustained for at least 4 weeks.
• Progressive disease (PD): ≥20% increase in the sum of the longest diameters compared to the smallest recorded value, or an absolute increase of ≥5 mm in lesion size, or the appearance of new lesions.
• Stable disease (SD): Neither sufficient shrinkage to qualify as PR nor sufficient increase to qualify as PD.
The efficacy evaluation for this patient was PR (Figure 1).
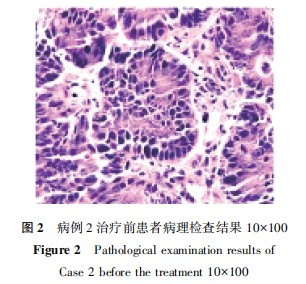
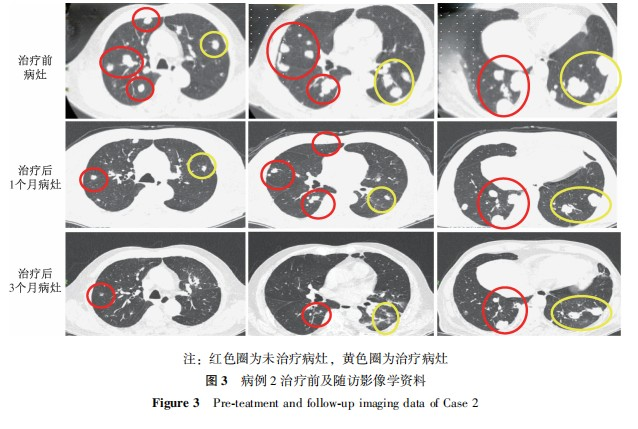
Case 2: A male patient, 81 years old, presented with the chief complaint of "multiple pulmonary metastases 6 months after colon cancer surgery." Positron emission tomography-computed tomography (PET-CT) showed: after right hemicolectomy, no obvious abnormal metabolism at the anastomotic site; multiple nodules of varying sizes in both lungs with increased metabolism, considered as metastases; an irregular hyperdense nodule in the right frontal subdural region with metabolism lower than the brain parenchyma and mild surrounding edema, possibly a meningioma. Chest CT indicated: multiple nodular masses in both lungs, some with cavitation, considered as metastatic tumors based on the medical history. After the condition was explained to the patient's family, a CT-guided lung biopsy was performed. Postoperative pathological examination of the lung biopsy tissue showed moderately differentiated adenocarcinoma, which, combined with the medical history, was considered most likely a metastasis after colon cancer surgery (Figure 2). The clinical diagnosis was secondary malignant tumor of the lung, ascending colon malignant tumor post-surgery, AJCC stage 8th edition T3N0M1a IV A. After multidisciplinary consultation, a treatment plan was formulated. After the condition was explained to the patient and his family, and with their informed consent, carbon ion therapy was administered under general anesthesia with high-frequency oscillatory ventilation control for some metastatic lesions in the left lung, with a dose of 50 Gy (RBE) in 1 fraction. The treatment process proceeded smoothly. Follow-up examinations at 1 month, 3 months, and 9 months after treatment showed that the treated lesions had significantly shrunk, with a therapeutic evaluation of PR. Other metastatic lesions in the lungs that were not irradiated also showed varying degrees of shrinkage (Figure 3).
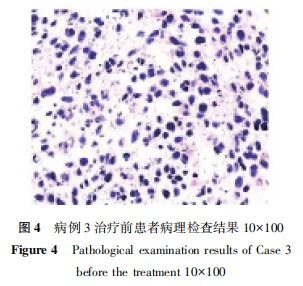
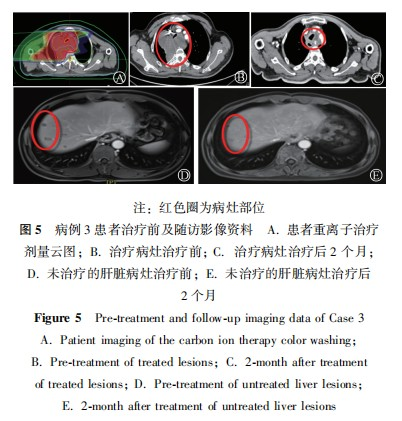
Case 3: A 53-year-old male patient presented with the chief complaint of "progressive dysphagia for 4 months and hoarseness for 1 month." Chest CT showed: after radical esophagectomy, multiple nodules and masses in the mediastinum, some of which were fused, suggestive of metastases. Upper abdominal magnetic resonance imaging (MRI) revealed: multiple nodular shadows in the liver with atypical lesion enhancement, and some nodules showed suspicious halo-like enhancement, raising the possibility of metastases. An ultrasound-guided biopsy of the mass behind the sternum was performed, and the pathology report showed: malignant tumor. Based on immunohistochemical results, the tumor was suspected to be of mesenchymal origin. Immunohistochemistry results were as follows: CK5/6 (−), CKp (−), Ki-67 (index approximately 50%), P40 (−), P63 (−), Vimentin (+), CR (−), HMB-45 (−), S-100 (−), SMA (focal +), Desmin (−), CD117 (−), DOG1 (−) (Figure 4). The patient was clinically diagnosed with: mediastinal malignant tumor (mesenchymal origin); secondary malignant tumor of the bone; secondary malignant tumor of the lymph nodes; secondary malignant tumor of the liver; esophageal malignant tumor (postoperative); squamous cell carcinoma. After multidisciplinary consultation, a treatment plan was formulated, and the patient's family was informed of the condition. With the patient's and family's informed consent, palliative carbon ion radiotherapy was administered to part of the mediastinal mass. The first course of treatment involved a dose of 30 Gy (RBE) in 10 fractions. After treatment, a follow-up CT scan showed significant shrinkage of the mass, and the compression of the trachea was improved compared to before. The second course plan was modified, with a target dose of 18 Gy (RBE) in 6 fractions. After communication with the family, carbon ion radiotherapy was administered to the metastatic lymph nodes in the left neck, with a total dose of 52.8 Gy (RBE) in 12 fractions. Carbon ion radiotherapy was also given to the metastatic lesion at the C3 vertebral body, with a total dose of 52.8 Gy (RBE) in 12 fractions. Carbon ion radiotherapy was administered to part of the metastatic lesion in the S8 segment of the liver, with a total dose of 66 Gy (RBE) in 10 fractions. Stereotactic ablative radiotherapy (SABR) was performed for the metastatic lesions in the right ilium and L5 vertebral body, with a total dose of 20 Gy in 5 fractions. The treatment process proceeded smoothly. After treatment, follow-up chest CT and abdominal MRI scans were performed. Based on RECIST 1.1 criteria, the therapeutic effect was evaluated as PR. Two months after treatment, a follow-up examination revealed that the untreated liver metastatic lesions had disappeared (Figure 5).
Ⅱ.Discussion
In 1953, Mole first proposed the concept of the abscopal effect during an abdominal irradiation experiment on rats [5,7]. In 1975, during radiotherapy for cutaneous reticulum cell sarcoma, the regression of metastatic tumors in non-irradiated areas was observed, and since then, subsequent literature has reported the phenomenon of the abscopal effect [8-12]. The abscopal effect refers to the shrinkage or even disappearance of tumor lesions in non-irradiated target areas during radiotherapy when a local tumor lesion is irradiated [13]. Relevant studies have reported that the mechanism of its occurrence may be that radiotherapy can activate the immune system, release tumor-associated antigens, increase the immunogenicity of the tumor microenvironment, thereby triggering a systemic anti-tumor immune response in the body, and causing a certain degree of growth inhibition of tumors outside the irradiated target area [13-15]. Of course, it is also possible that, in addition to directly killing tumor cells, local radiotherapy also induces immune cells to release pro-inflammatory cytokines, inducing chromosomal breaks or mutations in tumor cells outside the irradiated target area, thereby exerting an immune-mediated tumor-killing effect, resulting in the shrinkage or disappearance of tumors outside the irradiated target area [13].
In addition, the occurrence and development of the abscopal effect are also associated with radiation dose, fractionation mode, type of immunotherapy, and tumor type. In particular, tumor immunogenicity is an important factor in the occurrence of the abscopal effect [15-16]. Relevant studies have reported that proton, α-particle, and carbon ion radiotherapy can enhance tumor immunogenicity [15]. Carbon ion radiotherapy is the most ideal tumor radiotherapy technique in clinical radiotherapy. Compared with conventional photon radiotherapy, carbon ion therapy can induce a stronger tumor immune response [1]. In this study, after a thymic cancer patient received carbon ion therapy for one year, the untreated tumor outside the irradiated area significantly shrank. The thymus is an immune organ in the human body. Coupled with the physical and biological characteristics of carbon ions, such as high LET and higher RBE compared to photons, carbon ions are more capable of inducing a stronger immune response [2-4,17]. Demaria et al. [18] also mentioned in their study of the biological mechanism of radiotherapy-induced abscopal effect (AE) that immunodeficient mice do not exhibit the abscopal effect. Other studies have also shown that the mechanism of the abscopal effect is considered to be the result of a series of changes in the human immune system triggered by local radiotherapy [6]. Therefore, it can be considered that after thymic cancer patients receive carbon ion irradiation, the thymus, as an immune organ, acts as a mediator to enhance the presentation of tumor cell-associated antigens and improve the immune system's recognition of tumors, thereby making it easier to induce the abscopal effect [19]. Sharab et al. [20] also reported that hypofractionated radiotherapy and high-linear-energy-transfer (LET) radiation can increase the antigen presentation of tumor-associated antigens and T-cell recognition, thereby more easily inducing the abscopal effect.
In this study, for a patient with "colon cancer post-surgery and multiple lung metastases," a single high-dose carbon ion irradiation of 50 Gy (RBE) was administered to part of the metastatic lesions in the left lung. Subsequent follow-up examinations showed that the treated lesions were evaluated as partial response (PR), and the untreated lung lesions also showed varying degrees of shrinkage, indicating the occurrence of the abscopal effect. This is consistent with the research findings reported by Sharab et al. [20]. Among the cases observed in this study, the thymic cancer patients and the patient with mediastinal malignant tumor (mesenchymal origin) received multiple moderate radiation doses, while the patient with colon cancer post-surgery and multiple lung metastases received a single hypofractionated irradiation. All three patients experienced tumor shrinkage within 3 months after treatment, and the untreated tumors also shrank, exhibiting the abscopal effect. This effect persisted during subsequent follow-ups and was clearly observed on enhanced CT/PET-CT scans. This is consistent with research conclusions that lower radiation doses (1.8–2.0 Gy) are insufficient to trigger a strong immune response, moderate radiation doses (8–12 Gy) can enhance the immune response and induce a strong anti-tumor effect, but higher radiation doses (15–20 Gy) may reduce the occurrence of the abscopal effect. Hypofractionated radiation can induce strong immunogenicity, thereby facilitating the induction of the abscopal effect [21].
The three cases observed in this study did not receive any immunotherapy or other drug treatments during the treatment process. The occurrence of the abscopal effect was entirely due to carbon ions, and the possible mechanism is consistent with existing research conclusions. However, the sample size in this study was small. Whether the mechanism of action is due to the unique physical and biological advantages of carbon ions, the specificity of the immune system, the sensitivity of the tumor itself to radiation, or whether carbon ion therapy is more effective than photon therapy in inducing the abscopal effect, and whether the combination of immunotherapy can enhance the occurrence of the carbon ion-induced abscopal effect, requires further exploration and research.
In conclusion, carbon ions have advantages such as high LET, high RBE, and complex DNA damage. Compared with conventional radiotherapy, carbon ions have the potential to activate stronger immunogenicity in tumor cells [17]. Further exploration of the mechanism by which carbon ions induce the abscopal effect is of great significance for finding more effective treatments for tumor radiotherapy.
Conflict of Interest:None
Author Contributions:Qin Tianyan was responsible for data collation, analysis, and manuscript writing; Zhang Yihui and Pan Xin were responsible for guiding data analysis; Zhang Yanshan and Ye Yancheng were responsible for guiding manuscript writing; Wang Xin, Yang Yuling, Ma Tong, Lü Caixia, and Li Pengqing were responsible for data collection.
References
[1] Marcus D, Lieverse R, Klein C, et al. Charged particle and conventional radiotherapy: Current implications as partner for immunotherapy [J]. Cancers (Basel), 2021, 13(6):1468. DOI:10.3390/cancers13061468.
[2] 贾蓉, 苏锋涛, 胡步荣. 重离子的辐射生物效应及其在生命科学中的应用 [J]. 生物技术通报, 2018, 34(1):67-78. DOI:10.13560/j.cnki.biotech.bull.1985.2017-0735.
[3] Schmid TE, Multhoff G. Non-targeted effects of photon and particle irradiation and the interaction with the immune system [J]. Front Oncol, 2012, 2:80. DOI:10.3389/fonc.2012.00080.
[4] Keisari Y, Kelson I. The potentiation of anti-tumor immunity by tumor ablation with alpha particles, protons, or carbon ion radiation and its enforcement by combination with immunoadjuvants or inhibitors of immune suppressor cells and checkpoint molecules [J]. Cells, 2021, 10(2):228. DOI:10.3390/cells10020228.
[5] 高玉婷, 李媛, 金晓东. 碳离子辐射诱导的远隔效应 [J]. 生物化学与生物物理进展, 2023, 50(8):1915-1925. DOI:10.16476/j.pibb.2022.0371.
[6] Park B, Yee C, Lee KM. The effect of radiation on the immune response to cancers [J]. Int J Mol Sci, 2014, 15(1):927-943. DOI:10.3390/ijms15010927.
[7] Mole RH. Whole body irradiation: radiobiology or medicine? [J]. Br J Radiol, 1953, 26(305):234-241. DOI:10.1259/0007-1285-26-305-234.
[8] Matsubara S, Horiuchi J, Okuyama T, et al. A case of reticulu cell sarcoma of the skin showing abscopal effect during radiotherapy (author's transl) [J]. Nihon Igaku Hoshasen Gakkai Zasshi, 1975, 35(10):860-867.
[9] Togitani K, Asagiri T, Iguchi M, et al. Systemic abscopal effect of low-dose radiotherapy (2 Gy × 2) against palatine tonsil follicular lymphoma [J]. Intern Med, 2022, 61(20):3107-3110. DOI:10.2169/internalmedicine.8968-21.
[10] Sasaki H, Kato J, Horimoto K, et al. Delayed-onset abscopal effect after palliative radiotherapy for acral melanoma treated with anti-PD-1 therapy [J]. J Dermatol, 2022, 49(8):e255-e256. DOI:10.1111/1346-8138.16380.
[11] Zhang X, Zhang Y, Liu Y, et al. Stereotactic body radiotherapy-induced abscopal effect twice after pembrolizumab failure in hereditary leiomyomatosis and renal cell carcinoma: a case report with genetic and immunologic analysis [J]. Transl Androl Urol, 2021, 10(11):4304-4312. DOI:10.21037/tau-21-644.
[12] 丁心静, 卢致辉, 王芬, 等. 远隔效应在非小细胞肺癌免疫治疗时代的研究进展 [J]. 肿瘤预防与治疗, 2023, 36(5):432-439. DOI:10.3969/j.issn.1674-0904.2023.05.009.
[13] 张一贺, 张雁山, 李小军, 等. 碳离子治疗复发胸腺癌产生远隔效应临床观察1例 [J]. 中国肿瘤临床, 2021, 48(20):1075-1076. DOI:10.12354/j.issn.1000-8179.2021.20211145.
[14] 高怡凡, 孙晓蓉, 邢力刚. 放射免疫治疗中远隔效应的作用机制及临床应用 [J]. 中华肿瘤防治杂志, 2023, 30(14):881-886. DOI:10.16073/j.cnki.cjcpt.2023.14.09.
[15] 徐唐鹏, 胡梦雪, 许斌, 等. 远隔效应的作用机制及临床进展 [J]. 肿瘤学杂志, 2019, 25(3):202-205. DOI:10.11735/j.issn.1671-170X.2019.03.B005.
[16] Gorin JB, Ménager J, Gouard S, et al. Antitumor immunity induced after α irradiation [J]. Neoplasia, 2014, 16(4):319-328. DOI:10.1016/j.neo.2014.04.002.
[17] 高玉婷, 李鹏飞, 马国榕, 等. 辐射诱导远隔效应机制的研究进展 [J]. 中华放射肿瘤学杂志, 2023, 32(9):861-865. DOI:10.3760/cma.j.cn113030-20220822-00285.
[18] Demaria S, Ng B, Devitt ML, et al. Ionizing radiation inhibition of distant untreated tumors (abscopal effect) is immune mediated[J]. Int J Radiat Oncol Biol Phys, 2004, 58(3):862-870. DOI:10.1016/j.ijrobp.2003.09.012.
[19] 张惠博, 龚虹云, 刘华丽, 等. 远隔效应的研究进展与临床意义[J]. 肿瘤学杂志,2017,23(4):321-326. DOI:10.11735/j.issn.1671-170X.2017.04.B014.
[20] Sharabi AB, Nirschl CJ, Kochel CM, et al. Stereotactic radiation therapy augments antigen-specific PD-1-mediated antitumor immune responses via cross-presentation of tumor antigen [J]. Cancer Immunol Res, 2015, 3(4):345-355. DOI:10.1158/2326-6066.CIR-14-0196.
[21] Mortezaee K, Parwaie W, Motevaselei E, et al. Targets for improving tumor response to radiotherapy [J]. Int Immunopharmacol, 2019, 76:105847. DOI:10.1016/j.intimp.2019.105847.
