Using Spyglass for Diagnosis, ERCP, and Radical Surgery: A Case of Precision Treatment for Cholangio
Using Spyglass for Diagnosis, ERCP, and Radical Surgery: A Case of Precision Treatment for Cholangiocarcinoma
Cholangiocarcinoma is a relatively rare malignant tumor, accounting for less than 1% of all systemic tumors and about 3% of digestive system tumors. In recent years, its incidence has shown an increasing trend. It mostly affects people aged 50–70, with a male-to-female ratio of 1.4:1. It is classified into hilar cholangiocarcinoma and distal cholangiocarcinoma. Common causes include abnormal pancreatobiliary junction, biliary cysts/residual biliary cysts, recurrent pyogenic cholangitis, hepatolithiasis, postoperative biliary inflammation, primary sclerosing cholangitis, and viral hepatitis.
Early-stage cholangiocarcinoma often presents no obvious clinical symptoms. As the lesion progresses and enlarges, obstructive jaundice may occur due to biliary obstruction. With further progression, symptoms such as right upper quadrant pain, nausea, abdominal mass, vomiting, pale stools, dark urine, and itchy skin may appear. Cholangiocarcinoma is highly malignant, and early detection and diagnosis are challenging. Often, the disease is already advanced at diagnosis, leading to a poor prognosis.
Diagnosis requires a combination of clinical presentation, abdominal imaging, and pathological examination. Our hospital now employs endoscopic ultrasound and Spyglass (choledochoscopy) to enable earlier detection and more precise pathological examination, thereby improving diagnostic accuracy.
Case Study
A patient, Mr. Ma, sought medical attention in October 2022 due to "sudden upper abdominal distension and pain for 5 days." Abdominal MRI upon admission indicated: pancreatic thickening with heterogeneous enhancement, reduced enhancement signal in the pancreatic head, enlarged lymph nodes in the portal–caval venous space, suggesting possible tumor. Peripancreatic effusion and pancreatic duct dilation were observed, consistent with acute pancreatitis. Mild intra- and extrahepatic biliary dilation and stenosis of the pancreatic segment of the common bile duct were noted, along with multiple gallstones.
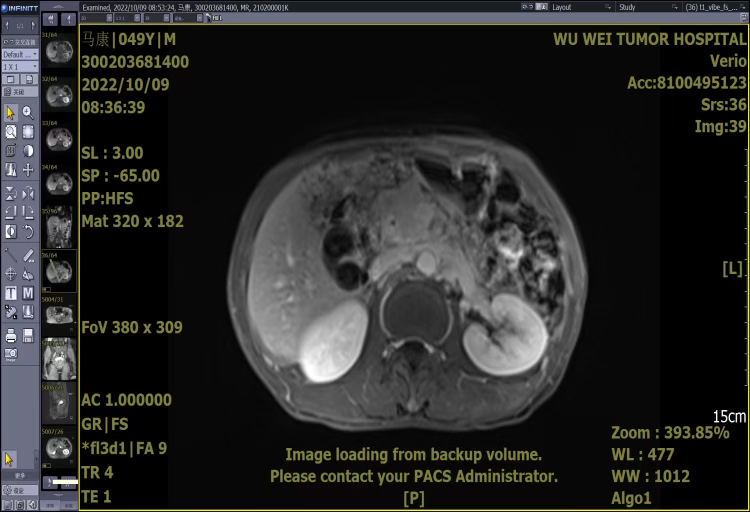
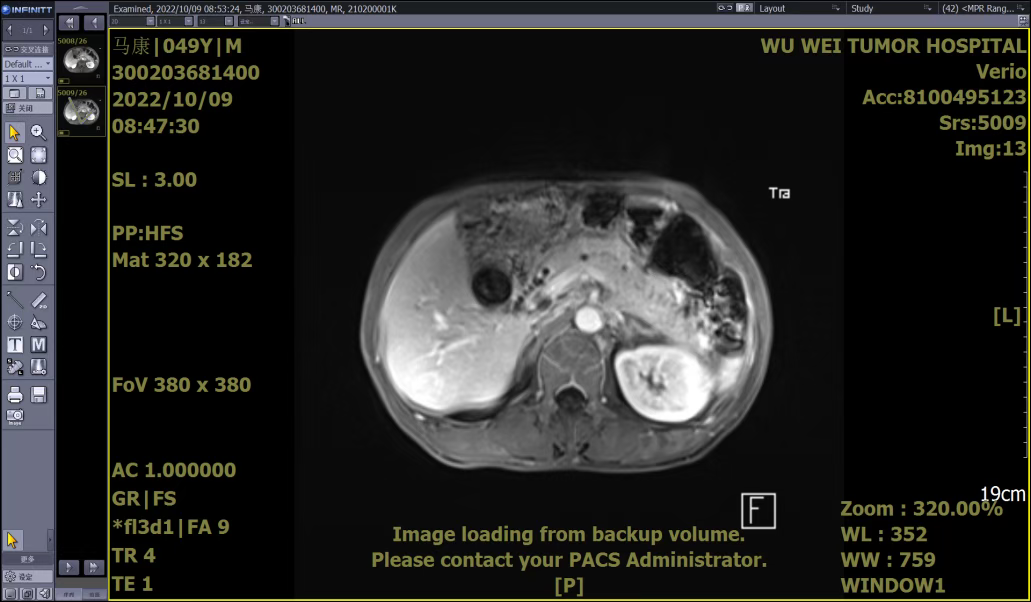
After admission, symptomatic treatments such as anti-infection therapy, enzyme inhibition, and fluid replacement were administered. Endoscopic retrograde cholangiopancreatography (ERCP) with nasobiliary drainage was performed. Endoscopic ultrasound revealed an irregular hypoechoic lesion in the pancreatic head, dilation of the main pancreatic duct, invasion of the pancreatic segment of the common bile duct, and a solid irregular lesion within the duct wall. An enlarged hypoechoic lymph node was observed near the portal vein. Pathological examination of the endoscopic ultrasound-guided pancreatic biopsy showed: (Pancreatic head puncture tissue) blood clot-like material with a small amount of pancreatic tissue, consistent with acute pancreatitis and necrotic changes.
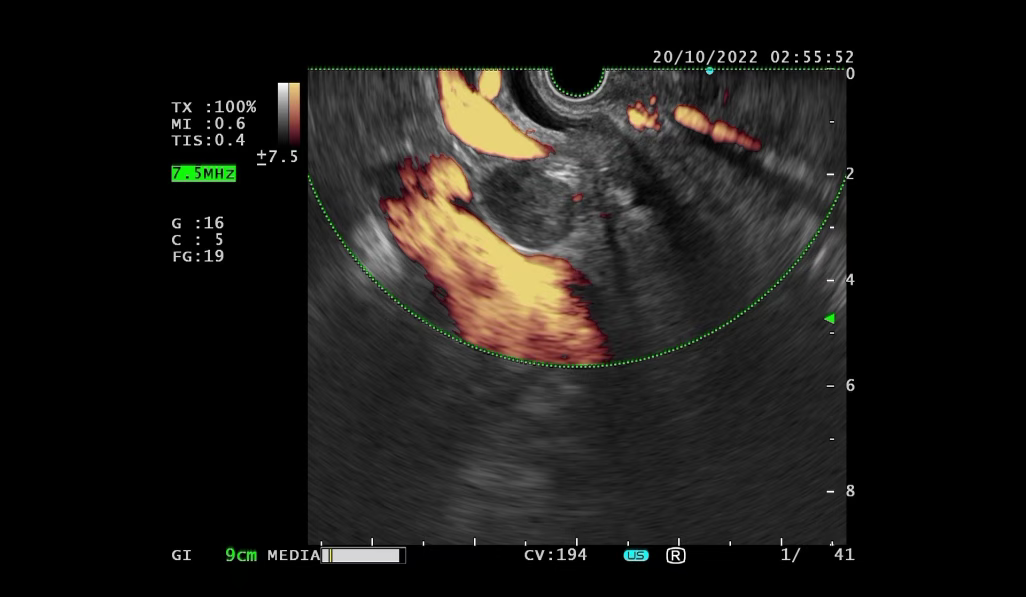
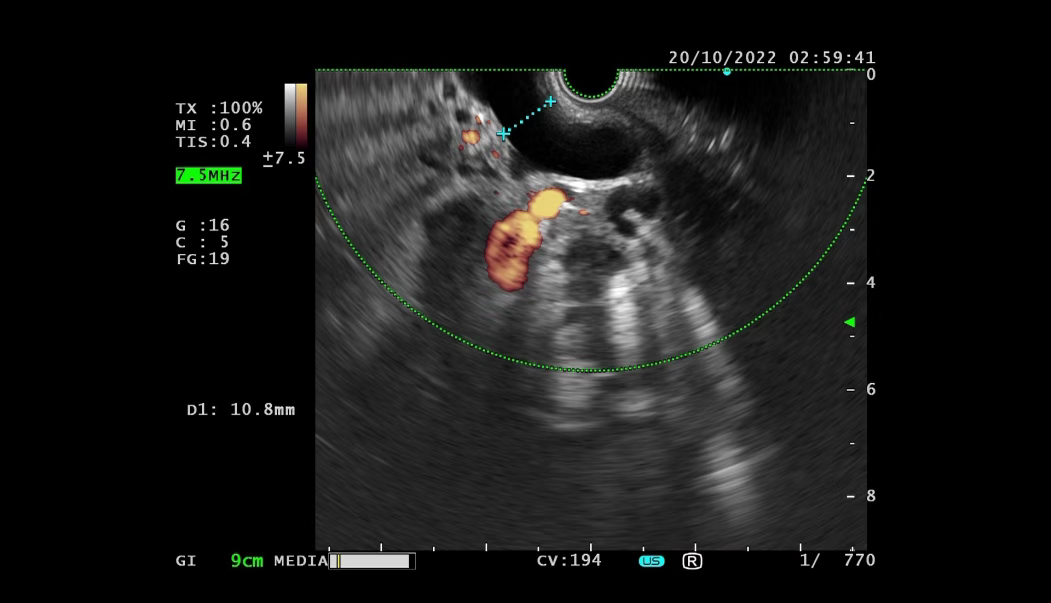
Although the initial biopsy did not support a tumor diagnosis, abdominal MRI and endoscopic ultrasound suggested possible invasion of the common bile duct and enlarged lymph nodes near the portal vein. To avoid misdiagnosis, Spyglass examination was performed. Spyglass choledochoscopy revealed destruction, hyperplasia, and diffuse stenosis in the middle and lower segments of the bile duct, with fragile tissue prone to bleeding. Pathological examination confirmed adenocarcinoma of the distal common bile duct.
The patient subsequently underwent preoperative chemotherapy followed by radical surgery for cholangiocarcinoma at our hospital.
This case highlights the significant diagnostic value of endoscopic ultrasound and Spyglass in identifying cholangiocarcinoma. The patient, initially presenting with abdominal pain and MRI findings suggestive of acute pancreatitis and enlarged portal vein lymph nodes, was ultimately diagnosed with cholangiocarcinoma through advanced endoscopic techniques.
Introduction to the Department of Gastroenterology, Wuwei Medical Science Academy
The Department of Gastroenterology is a Gansu Provincial Key Discipline, a demonstration base for the national major public health service project "Early Diagnosis and Early Treatment of Upper Gastrointestinal Cancer" under the Rural Cancer Early Diagnosis and Early Treatment Program, a training base for endoscopic professionals in gastroenterology designated by the National Health Ministry, the Gansu Provincial Key Laboratory of Gastrointestinal Diseases, the Wuwei Sub-center of the Chinese Helicobacter pylori Molecular Medical Center, and the Wuwei Branch of the Xijing Biobank, among other designations.
The department boasts a professional team led by a large number of experts with senior professional titles, including Zhang Zhiyi, Chief Physician, a leading talent in the Gansu provincial health system and the municipal leading talent of Wuwei, founder of the Department of Gastroenterology at Wuwei Medical Science Academy Tumor Hospital, and Director of the Gastroscopy Center; Nie Peng, Chief Physician, Assistant to the President (Master of Medicine); Chief Physicians Lu Linzhi and Zhang Wenhong (Master of Medicine); Deputy Chief Physicians Zhao Guangyuan (Master of Medicine), Li Shihua, Liu Jindian (Master of Medicine), and Xie Chunfang.

The Department of Gastroenterology is equipped with over 300 various pieces of equipment, including the first domestically produced four-arm surgical robot, the fourth PET-CT in Gansu province and the first among prefectural-level city hospitals in the province, a dynamic 500-slice gemstone spectral CT, and an Optima670 64-row 128-slice spiral CT; more than 10 various types of laparoscopes, including STORZ·HD full HD laparoscopes, HD 3D thoracic laparoscopes, and HD 3D fluorescent laparoscopes; and over 30 endoscopes, including Olympus NBI magnifying endoscopes and ultrasonic endoscopes.
Spotlight on Gastroenterology

The Charisma of the Heavy Ion Campus

Department Overview
The First Department of Gastroenterology at Wuwei Medical Science Academy Heavy Ion Hospital currently has 1 Chief Physician, 2 Associate Chief Physicians, 2 Attending Physicians, and 3 Resident Physicians. The Chief Physician, Lu Linzhi, is a Longyuan Youth Innovative Talent, Vice Chairman of the Gastroenterology Professional Committee of the Wuwei Medical Association, a member of the Gastroenterology Professional Committee of Integrated Medicine in Gansu Province, and an honoree of the Wuwei "Tianma Craftsman" title. She specializes in the early diagnosis, treatment, and clinical research of gastrointestinal tumors. The department routinely performs gastroscopy and colonoscopy, EMR (Endoscopic Mucosal Resection), ESD (Endoscopic Submucosal Dissection), EUS (Endoscopic Ultrasonography) and puncture and treatment techniques under ultrasonic endoscopy, ERCP (Endoscopic Retrograde Cholangiopancreatography), POEM (Peroral Endoscopic Myotomy), STER (Submucosal Tunneling Endoscopic Resection), gastrostomy, pancreatic tumor particle implantation, and esophageal and intestinal stent placement.

Contact Us
Hotline: 0935-6989302, 0935-6989301
Hospital Address: First Floor, Building 3, Heavy Ion Hospital District, Wuwei Medical Science Academy Tumor Hospital, Gansu Province
Preliminary Review: Zhang Lihong
Final Review: Zhang Jie
