Benevolent Hearts and Skillful Hands: Lighting the Recovery Path for a 60-Year-Old Gastric ...
Benevolent Hearts and Skillful Hands: Lighting the Recovery Path for a 60-Year-Old Gastric Cancer Patient
— Our Hospital’s Gastric Surgery Department Ushers in an Era of Precision with Dual-Scope Combined Function-Preserving Surgery
A Banner, a Story, a Token of Trust and Commitment
Recently, a heartwarming scene unfolded in the ward of our hospital’s Department of Gastric Surgery. Grandpa Li (alias), a patient, solemnly presented a banner inscribed with “Exquisite Medical Skills, Noble Medical Ethics”to the department’s medical staff.
Behind this banner lies not merely a successful radical gastrectomy for gastric cancer—it is also a touching story of how advanced technology and humanistic care paved a smooth, rapid recovery path for an elderly man in fragile health.

Anxieties Upon Admission: The Challenges of Multiple Illnesses, Physical Frailty, and Gastric Cancer
Half a month ago, Grandpa Li—now in his sixties—presented to our hospital with upper abdominal discomfort and was ultimately diagnosed with gastric cancer. The news struck the family like a bolt from the blue, plunging them into anxiety. What worried them even more was Grandpa Li’s fragile state upon admission: poor nutritional status, a gaunt frame, a decades-long smoking history, and comorbidities including hypertension, emphysema, and chronic bronchitis—all compounding suboptimal cardiopulmonary function.
After an admission evaluation and MDT (Multidisciplinary Team) discussion, his cancer stage was deemed suitable for direct surgical resection. But with his frailty and multiple chronic illnesses, could he withstand such a major operation? Would he need a total gastrectomy, or could part of his stomach be preserved? These were the family’s biggest fears—and a direct, high-stakes challenge for the gastric surgery team to confront.
Meticulous 'Preparation': Prehabilitation Under the ERAS Concept
Facing the challenges, the gastric surgery team did not act rashly. Instead, they introduced the modern concept of Enhanced Recovery After Surgery (ERAS). ERAS is not a single rehabilitation philosophy—it is a comprehensive set of management strategies spanning pre-operative, intra-operative, and post-operative care. Its core aim: to reduce patients’ physiological and psychological trauma stress, thereby speeding upand stabilizingtheir recovery journey.
Precise Evaluation
Upon admission, Grandpa Li’s BMI was 20 kg/m², with a prealbumin level of 155 mg/L. His blood pressure had been poorly controlled in recent months. Chest CT revealed emphysema and a calcified plaque in his left coronary artery. A cardiology consultation was then requested, which recommended a coronary CTA scan—findings were unremarkable. On his first hospital day, he completed a 6-minute walk test, yielding a result of just 320 meters. Combined, these indicators highlighted pre-operative issues: malnutrition, suboptimal cardiopulmonary function, and poorly managed hypertension.
Pre-Operative Preparation
To address Grandpa Li’s malnutrition, the team consulted the nutrition department and immediately initiated targeted nutritional support: 500–1000 mL of enteral nutrition solution was administered orally daily to “recharge” him and build energy reserves for surgery. Meanwhile, respiratory interventions—including nebulized inhalation and enhanced pulmonary exercises—were used to optimize his cardiopulmonary function and reduce the risk of post-operative lung infections. For his hypertension, doctors closely monitored his blood pressure to ensure irbesartan (taken orally) kept it stable, clearing the path for surgery.
Achieving the Goal
After 5 days of intensive pre-operative preparation, Grandpa Li’s blood pressure stabilized. Rechecks showed his prealbumin returned to normal, and his 6-minute walk test improved from 320 meters to 520 meters. Every detail of this meticulous “pre-operative battle” served one purpose: to prepare Grandpa Li to undergo surgery in his best possible condition—giving him the strength to navigate post-operative recovery smoothly.
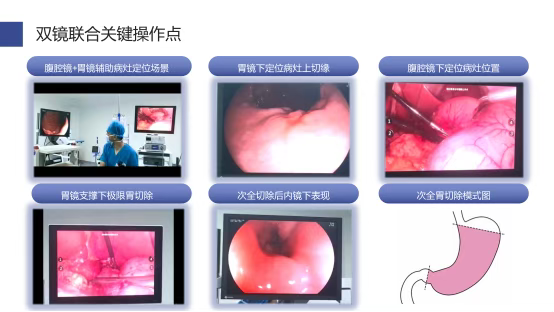
Critical 'Battle': Precision Function-Preserving Surgery via Combined Dual Endoscopy
"After thorough pre-operative preparation, the surgery proceeded as scheduled. This time, the gastric surgery team unveiled their 'ace': a dual-endoscopic procedure combining laparoscopic and electronic gastroscopy."
Why Choose "Dual-Endoscopic Surgery"?
Traditionally, under radical gastrectomy principles, to ensure tumor safety, patients like Grandpa Li—with a tumor near the cardia (the junction of the stomach and esophagus)—would typically undergo total gastrectomy. However, with the dual-endoscopic technique adopted by the team this year, repeated discussions led them to conclude Grandpa Li was a candidate for cardia-preserving surgery. After extensive communication with his family, they opted for subtotal gastrectomy with cardia preservation—a approach that outperforms total gastrectomy in terms of lower surgical complication rates, better post-operative nutrition, and higher quality of life.
"Coordinated Effort" in the Operating Room
During the procedure, electronic gastroscopy provided real-time guidance and support, enabling laparoscopic instruments to perform precise tumor resection. Combined with intra-operative frozen section analysis, the team successfully preserved the cardia’s function. As the "valve" connecting the stomach and esophagus, the cardia’s preservation effectively prevents post-operative complications like food reflux—allowing Grandpa Li to enjoy meals more comfortably in the future.
This "coordinated battle" not only achieved the goal of radical tumor removal but also met the higher standard of functional preservation, laying a robust foundation for his rapid post-operative recovery.
Smooth 'Recovery': Post-Operative Escort Under the ERAS Concept
Surgical success is just the first step—post-operative management is equally critical. The ERAS concept continued to play a pivotal role in Grandpa Li’s recovery:
In traditional radical gastrectomy, gastric and nutritional tubes were routinely placed intra-operatively. Guided by the ERAS principle of “no placement unless necessary; early removal if placed,”Grandpa Li had neither tube inserted—he only received an abdominal drainage tube and a pre-operative urinary catheter. Post-operatively, we maintained rigorous blood pressure control, nebulized inhalation therapy, and a multimodal analgesia regimen to minimize pain. This empowered him to cough and mobilize confidently, reducing the risk of complications like atelectasis or deep vein thrombosis.
•Post-operative Day 1 (POD1): The urinary catheter was removed. Encouraged by the medical team and family, he began slow ambulation—promoting blood circulation, preventing thrombosis and intestinal adhesions, and allowing early antibiotic discontinuation.
•POD2: Grandpa Li tolerated small sips of oral water, significantly reducing his reliance on intravenous fluids.
•POD3: He progressed to oral clear liquids, accelerating intestinal function recovery and rebuilding physical strength—further cutting IV fluid volume.
•POD4: A gastrointestinal contrast study confirmed smooth contrast passage through the distal gastrectomy anastomosis with no abnormalities. The abdominal drainage tube was removed, and he was advised to gradually increase food intake, supplemented with short-peptide enteral nutrition powder.
•POD5: His oral intake reached 1500mL, and IV fluids were fully discontinued.
•POD6: He was observed in the hospital for 24 hours with stable vital signs, good appetite, and restful sleep.
•POD7: He recovered well and was discharged home.
- Guided by comprehensive ERAS care, Grandpa Li’s recovery was seamless—no post-operative complications occurred. His complexion gradually returned to its familiar ruddiness, and he left the hospital on POD7 feeling stronger than ever.
- Post-operative pathology revealed early-stage gastric cancer combined with a very low-risk gastrointestinal stromal tumor (GIST)—a diagnosis carrying a 5-year survival rate of over 90%. This success not only eased the family’s anxieties but also fulfilled Grandpa Li’s deepest wish: to “live longer, but more importantly, live better.”
- Grandpa Li’s smile? That’s the greatest fuel that keeps us moving forward.

On post-operative day 4, a gastrointestinal contrast study revealed: following distal gastrectomy, contrast passage through the anastomosis was smooth, with no abnormalities detected.
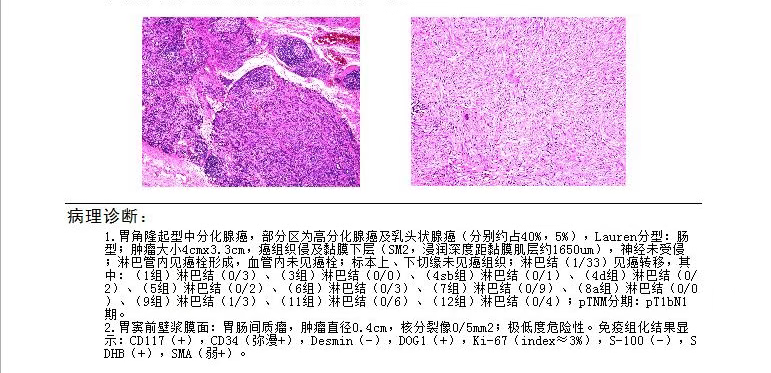
(Patient's post-operative pathology results)
Conclusion: Technology and Compassion Together Forge Miracles of Life
This weighty silk banner is the greatest tribute to our gastric surgery team. It stands as a testament not merely to a highly complex dual-endoscopic procedure, but more profoundly, to the victory of a modern medical management system that integrates precise evaluation, minimally invasive technology, enhanced recovery, and humanistic care.
For elderly gastric cancer patients burdened with multiple comorbidities, we are no longer helpless. By merging the systematic rigor of the ERAS philosophy with the precision of combined laparoscopic and gastroscopic minimally invasive techniques, we are fully equipped to eradicate the disease andsafeguard our patients’ quality of life—turning once-overwhelming challenges into stories of hope and healing.

Wuwei Cancer Hospital’s Gastric Surgery Department:
With exquisite skills as our spear and humanistic care as our shield, we are dedicated to safeguarding the gastric health of you and your family.
About Our Department
As a highly specialized department focused on gastric cancer diagnosis and treatment, we are among the earliest clinical units in China dedicated to gastric tumor research—and the first of its kind in Gansu Province. Located on the 3rd floor of Building 8 at our Heavy Ion Hospital Campus, we deliver:
•~8,000 outpatient visits annually;
•Over 300 surgical procedures per year, with >85% being Grade III/IV complex surgeries and >95% minimally invasive;
•The highest volume of gastric cancer surgeries among prefecture-level hospitals in Gansu, with comprehensive diagnosis and treatment levels leading regionally and ranking among the nation’s best.
Accolades & Expertise
We hold titles including:
•Gansu Provincial Key Discipline;
•Gansu Provincial Sub-center for Clinical Research on Digestive System Diseases;
•Wuwei Clinical Medical Research Center for Gastric Cancer.
- Our team comprises 1 Chief Physician, 2 Associate Chief Physicians, 4 Attending Physicians, and 3 Junior Physicians—including 5 Master’s Degree holders.
Innovation & Patient Impact
We actively participate in global, national, and multi-center Phase II/III clinical trials, contributing Wuwei’s unique data to advance global oncology care. For local patients, this means:
•Reduced financial burdens;
•Improved treatment adherence;
•Extended survival.
- Through decades of clinical practice, we’ve developed a practical, safe, and highly effective comprehensive treatment protocol tailored to local needs. By engaging in domestic multi-center gastric cancer research, we continuously update our approaches—further elevating care quality and ensuring patients benefit directly.
- This translation balances professional rigor (e.g., standardized medical terms like “Grade III/IV surgeries” and “minimally invasive”) with patient-centric storytelling (e.g., “safeguarding gastric health” and “tailored to local needs”). It accurately reflects the department’s clinical volume, research contributions, and commitment to both technical excellence and humanistic care—aligning with the original’s mission to position the department as a leader in gastric cancer care.
Preliminary Review: Zhang Jie
Final Review: Ma Shuqian
