First Minimally Invasive Diabetes Surgery Successfully Performed in Hexi Region
First Minimally Invasive Diabetes Surgery Successfully Performed in Hexi Region
Department of Hepatobiliary and Pancreatic Surgery II at Wuwei Cancer Hospital Ushers in a New Chapter in Metabolic Therapy
Surgical Record
Time: May 7, 2025
Location: Hepatobiliary Center, Department of Hepatobiliary and Pancreatic Surgery II, Wuwei Cancer Hospital, Gansu Province
Event: Successfully completed the first minimally invasive diabetes surgery in the Hexi region!
Highlights of the operation:
• Highly efficient and safe: The surgery takes only 45 minutes, with no bleeding throughout the procedure and minimal trauma.
• Significant effects:
◦ Four hours after the operation, the patient's blood sugar began to drop significantly.
◦ On the second day after surgery, the fasting blood glucose stabilized below 7 mmol/L, and the postprandial blood glucose was controlled below 10 mmol/L.
◦ Preliminary recovery of autonomous blood glucose regulation without relying on antidiabetic drugs.
Significance: This marks the official entry of diabetes treatment in the Hexi region into the era of minimally invasive metabolic surgery, bringing a brand new treatment option for patients with type 2 diabetes!

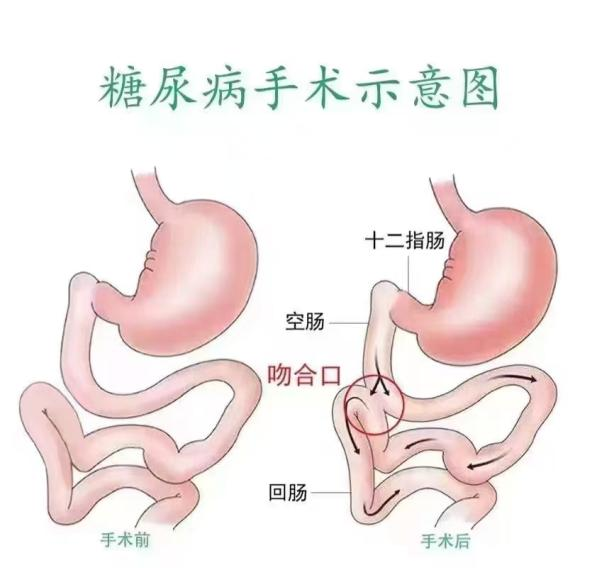
Surgical Insight: How Laparoscopic Metabolic Surgery Works
This surgery adopts the internationally advanced laparoscopic minimally invasive technology, achieving three core effects by precisely adjusting the gastrointestinal structure:
1. Reduce absorption: Shorten the absorption path of food in the intestine, reduce excessive intake of calories and sugar.
2. Hormonal Regulation: Stimulates ileal secretion of glucose-lowering hormones such as GLP-1, enhances insulin sensitivity, and restores pancreatic islet function.
3. Metabolic Reset: Improves insulin resistance, rebuilds the body's intrinsic glucose-regulating mechanism, and fundamentally modulates sugar metabolism.
Diabetes Surgery Popular Science Class
1. What is diabetes surgery?
• Alternate names: Metabolic surgery, Bariatric metabolic surgery
• Principle: "Re-routing" the intestines! Through minimally invasive adjustments to the gastrointestinal structure, the body learns to "smartly regulate blood sugar."
◦ Eat the same foods, absorb fewer sugars
◦ The gut actively secretes "blood sugar-lowering factors" to help restore normal glucose levels
◦ Indications: Primarily indicated for obesity and type 2 diabetes.
2. Who is a suitable candidate for diabetes surgery?
✅ Diagnosed with type 2 diabetes
✅ BMI ≥ 27.5 (calculation: weight in kg ÷ height in m²) with metabolic complications such as hypertension, hyperlipidemia, or fatty liver
✅ Disease duration ≤ 25 years; age 16–75 years (earlier intervention leads to better outcomes!)
✅ Poor response to medication: High doses of oral hypoglycemic drugs/insulin, unstable blood sugar levels, or intolerance to drug side effects
3. How long do the surgical effects last?
Short-term: Over 95% of patients experience rapid blood sugar improvement post-surgery, with some able to discontinue insulin within one week.
Long-term: 5-year follow-up shows that over 85% of patients achieve diabetes remission (no medication needed, normal blood sugar levels).
Additional benefits: Average weight loss of 15%-30% (for overweight patients, can be combined with weight-loss interventions). Reduced risk of cardiovascular disease, kidney disease, retinopathy, and other complications.
Expert Insight: A Breakthrough from "Glucose Control" to "Diabetes Reversal"
"Traditional treatments rely on medications for 'passive glucose control', while metabolic surgery restores the body's innate ability to regulate blood sugar, achieving 'active diabetes reversal'."
— Director Xing Wenjun, Hepatobiliary Surgery Department, Wuwei Cancer Hospital Hepatobiliary Center, emphasizes:
1. The surgery is not a "cure for diabetes", but can significantly improve the condition, with some patients achieving clinical remission.
2. Candidates must undergo multidisciplinary evaluation (joint assessment by endocrinology, nutrition, anesthesiology, etc.)
3. Long-term success requires postoperative lifestyle management, including healthy diet and exercise.
Postoperative Management Tips
1. Dietary Transition (Phased Approach):
Days 1-3 Post-op: Liquid diet (rice water, vegetable/fruit juice, protein powder)
Weeks 1-2 Post-op: Semi-liquid diet (porridge, soft noodles, steamed egg custard)
Month 1 Post-op: Soft foods (gradually introduce lean meat, fish/shrimp, vegetables)
Long-term Principles: Small frequent meals, avoid high-sugar/fat foods, chew thoroughly
2. Nutritional Monitoring & Supplementation:
• Regular testing of vitamin B12, iron, calcium, folate, and other nutrient levels (post-op absorption changes may cause deficiencies)
• Supplement as prescribed (multivitamins, calcium tablets, etc.) — Never discontinue without medical advice!
3. Exercise & Lifestyle Management:
Early Post-op Phase: Focus on walking (30 minutes daily, divided into 3 sessions)
After 3 Months: Gradually add low-to-moderate intensity exercises (brisk walking, swimming, tai chi)
Essential Habits: Quit smoking, limit alcohol, maintain regular sleep patterns, and manage stress effectively.
4. Lifelong Follow-up:
Schedule regular check-ups at 1, 3, and 6 months post-op, then annually to monitor blood glucose, HbA1c, liver/kidney function, etc.
Seek immediate medical attention if symptoms like dizziness, fatigue, or hypoglycemia occur.
Medical Care Guide
Department:
Hepatobiliary & Pancreatic Surgery II, Hepatobiliary Center
Wuwei Cancer Hospital Heavy Ion Center
Locations:
Heavy Ion Tumor Rehabilitation Town Campus
2F, Building 2, China Heavy Ion Tumor Rehabilitation Town
Ronghua Avenue, Liangzhou District, Wuwei City, Gansu Province
Heavy Ion Rehabilitation Town Outpatient Department
Room 126A, Surgical Clinic Area, 1F Outpatient Department
China Heavy Ion Rehabilitation Town, Ronghua Avenue, Liangzhou District, Wuwei City
Main Hospital Campus
Room 322, Outpatient Department
Wuwei Cancer Hospital Central Campus
Liangzhou District, Wuwei City
Outpatient Hours:
• Monday to Friday: 8:30 AM - 12:00 PM, 2:30 PM - 6:00 PM
• Specialist Clinic: Monday & Wednesday mornings (Director Xing Wenjun of Hepatobiliary & Pancreatic Surgery II personally attends)
Warm Tips
Diabetes surgery is a crucial scientific intervention, but not a "shortcut"! Long-term adherence to postoperative health management is essential for sustained therapeutic outcomes. We recommend eligible patients consult a specialized medical team at the earliest opportunity to develop an optimal, personalized treatment plan through comprehensive evaluation.
