Beyond the Stomach, A New Chapter Compassionate Skill, A Lasting Legacy
Beyond the Stomach, A New Chapter Compassionate Skill, A Lasting Legacy
—2025 Annual Report of the NIE Peng Surgical Team, Department of Gastric Surgery, Gansu Wuwei Cancer Hospital
Time passes and new chapters unfold. Looking back on 2025, the Department of Gastric Surgery at Gansu Wuwei Cancer Hospital advanced like a ship breaking through waves, sailing steadfastly across the vast ocean of medicine. United in purpose, with scalpels as our pens and compassion as our ink, we continued to write brilliance on the canvas of life.
This year, we continued to deepen our focus on gastric cancer diagnosis and treatment. We performed over 240 gastrointestinal surgeries, maintaining a consistent volume of over 200 procedures specifically for gastric cancer. Minimally invasive techniques were employed in over 90% of cases, with robotic surgery steadily advancing. Our postoperative complication rate remained strictly below 2%.
Our commitment to research and innovation bore significant fruit. Provincial key R&D projects and the Wu Jieping Medical Foundation project were successfully implemented, further elevating our academic influence. Clinical research progressed solidly, with multiple trials offering new hope to patients.
We were honored to be designated the "Chair Unit of the Tumor Minimally Invasive Therapy Committee of Gansu Anti-Cancer Association," leading the development of regional minimally invasive surgery. We actively advanced new techniques, including dual endoscopic stomach-preserving surgery, single-port thoracoscopic-assisted laparoscopic radical surgery for esophagogastric junction cancer, hyperthermic intraperitoneal chemotherapy (HIPEC), and metabolic/bariatric surgery, bringing new light to more patients.
Looking ahead to 2026, we will remain true to our founding mission of "Mastering Medicine with Virtue, Serving the World with Benevolence." We will forge ahead courageously on the path of gastric cancer prevention and treatment, driven by technological innovation and centered on patient well-being, to write a new chapter of high-quality development for our department.
As we reflect on the past, we have also selected a few memorable highlights from our team's work to share with you!
I. Navigating the Research Seas, Anchoring the Frontier:
Building the Foundation of a Scientific Research System, Driving Development Through Innovation
On the towering peaks of medical advancement, each breakthrough in targeted therapy and every innovation in treatment embodies the relentless, round-the-clock pursuit of explorers. This year, under the leadership of our discipline leader, Chief Physician Nie Peng, the Gastric Surgery team is making steadfast strides, leaving a determined and enduring mark in the field of life and health through unwavering scientific research.
We are delighted to witness key progress in the team's research project approvals: the Gansu Provincial Key Research and Development Project, Strategy and Mechanism Research on Heavy Ion Radiotherapy Sensitizing Gastric Cancer Treatment by Targeting the DNA Damage-Immune Rhythm Axis, and the Wu Jieping Medical Foundation Project, A Phase Ib/II Clinical Study of Low-Dose Radiotherapy Combined with Serplulimab and SOX Regimen as Neoadjuvant Therapy for Locally Advanced Gastric or Esophagogastric Junction Adenocarcinoma, have been approved successively. This not only recognizes our prior work but also provides robust support for our future in-depth exploration.
Seizing this opportunity, the department has fully launched the Gastric Cancer Series Research Project—the GARNET Study (Gastric Cancer Advanced Research for Neoadjuvant and Exploratory Therapeutics). Currently, four sub-studies have set sail with full momentum: ranging from multimodal exploration of neoadjuvant therapies (covering conventional photon radiotherapy, cutting-edge heavy ion radiotherapy, chemotherapy, and immunotherapy combinations) to innovative exploratory research on function-preserving surgical techniques, and further extending to in-depth basic research related to gastric cancer. These initiatives systematically encompass the fundamental mechanisms, clinical diagnosis, comprehensive treatment, and prognosis evaluation of gastric cancer, constructing a comprehensive, multidimensional scientific research matrix.
The core driving force behind all this stems from our unwavering belief: to build a research-oriented team centered on inquiry and guided by clinical challenges. We deeply understand that genuine medical advancement is rooted in the continuous questioning and validation that spans from the laboratory bench to the patient's bedside. Every sample analyzed, every piece of data accumulated, and every treatment protocol optimized represents a step toward finding a brighter, more precise path to life for gastric cancer patients.
The road ahead is long, and there is no end to innovation. The Gastric Surgery team will continue to pool wisdom and strength, wielding scientific research as our tool for dedicated exploration. We are committed to translating cutting-edge discoveries into tangible clinical benefits, contributing our professional expertise to the ongoing challenge of conquering gastric cancer.
II. Leading the Wave as the Committee Chair for Minimally Invasive Surgery:
Empowering Through Platform Outreach, Renewing the Academic Landscape
On the afternoon of October 17, 2025, the inaugural meeting of the First Committee of the Tumor Minimally Invasive Therapy Committee of the Gansu Anti-Cancer Association was grandly held at the Heavy Ion Center of Gansu Wuwei Cancer Hospital. During the meeting, Chief Physician Nie Peng, Vice President of Gansu Wuwei Cancer Hospital, was elected as the inaugural Chairperson. Fan Yong, Lu Linzhi, Wang Ji, Wei Dengwen, and Hu Ming were elected as Vice Chairpersons. The elected Standing Committee Members are Xu Ming, Zhu Duojie, Qiu Zhisheng, Yang Yonglin, Wang Yun, Zhang Yong, Lu Wenjun, Wang Jihong, Liao Jiangtai, Ren Guorong, Liu Yue, Zhang Tiancai, Shi Quanye, Zhang Xiaoru, and Zhang Zhenming. Wang Yongjin was appointed as Secretary-General, and Liu Xingji as Work Secretary.


The Gansu Anti-Cancer Association formally awarded Gansu Wuwei Cancer Hospital the designation of "Chair Unit of the Tumor Minimally Invasive Therapy Committee." This marks the first provincial-level medical committee platform to be undertaken by a prefectural/city-level hospital since the implementation of the Gansu Province Implementation Plan for Promoting the Expansion of High-Quality Provincial Medical Resources" in 2023. This move breaks from the traditional academic hierarchy defined by "city status" and establishes a new mechanism that prioritizes "technological prowess as the measure of standing."


This meeting signifies the official establishment of the province's first provincial-level academic organization for tumor minimally invasive therapy at a prefectural/city hospital. It represents a historic breakthrough, shifting the chair unit of a provincial committee from being exclusively "held by" top-tier hospitals in the provincial capital to being "taken over" by leading prefectural/city hospitals. This is not only a vivid example of the expansion and outreach of high-quality provincial medical resources but also a living benchmark for prefectural/city hospitals breaking through the "glass ceiling" and achieving leapfrog development. Taking this appointment as the chair unit as a new starting point, Gansu Wuwei Cancer Hospital will continue to amplify its technical advantages, accelerate the expansion and outreach of high-quality resources, contribute minimally invasive expertise to the building of a "Healthy Gansu," and write a heartening chapter in the rise of grassroots healthcare.
III. Dual Endoscopy in Concert, Preserving the Crucial:
Precise Eradication of Lesions, Maximizing Functional Preservation
With the continuous advancement of medicine, gastric cancer treatment has entered a new phase of "precision, minimally invasive, and function-preserving." Following this trend, our hospital has consistently stayed at the forefront, actively exploring more optimized and patient-friendly treatment plans, dedicated to preserving patients' quality of life to the greatest extent while curing the disease.
Ms. Yang, a 54-year-old patient, was diagnosed with early-stage gastric cancer during a routine health check-up. To achieve the dual goals of "curing the tumor" and "preserving function," the multidisciplinary team (MDT) from our hospital's Gastroenterology and Gastric Surgery departments collaborated closely to successfully perform a combined endoscopic and laparoscopic radical gastrectomy. During the surgery, the Gastroenterology team acted as "precision navigators," using the high-definition view of the gastroscope to clearly mark the tumor boundaries and achieve precise lesion dissection. The Gastric Surgery team served as the "minimally invasive lead surgeons," completing lymph node dissection and partial gastrectomy through just a few small ports using laparoscopic techniques. The entire procedure lasted only two hours, thoroughly removing the tumor while maximizing the preservation of healthy gastric tissue and function. Ms. Yang recovered smoothly after surgery, was able to consume liquid diets three days later, and was discharged for rehabilitation one week later. Since the beginning of this year, our department has successfully collaborated with the Gastroenterology team to complete over ten such dual endoscopic-laparoscopic combined surgeries.


The success of such surgeries marks an important shift for our hospital in the field of early gastric cancer treatment, moving from "solely focusing on radical cure" to "emphasizing both cure and quality of life." The dual endoscopy combined technique integrates three core advantages:
1. Precise Localization: The endoscope enables millimeter-level marking of the lesion, providing clear guidance for the laparoscopic surgery and ensuring thorough and accurate tumor removal.
2. Minimally Invasive Radical Resection: Laparoscopy offers a wide field of view and precise operation, resulting in minimal trauma, reduced bleeding, less patient pain, and a faster recovery.
3. Functional Preservation: This approach overcomes the limitations of traditional surgical methods, preserving normal gastric anatomy as much as possible and effectively maintaining the patient's postoperative digestive function and nutritional status.
All of this is rooted in our hospital's consistently patient-centered, multidisciplinary team (MDT) diagnostic and treatment model. The seamless collaboration between medical and surgical specialists has established a standardized pathway of "precise localization → minimally invasive resection → functional preservation," fully demonstrating our hospital's technical strength and teamwork capabilities in the comprehensive diagnosis and treatment of gastrointestinal tumors.
IV. Single Port, Ingenious Access to Resolve Complexities:
Tackling High-Position Tumors, Pioneering New Paths in Minimally Invasive Surgery
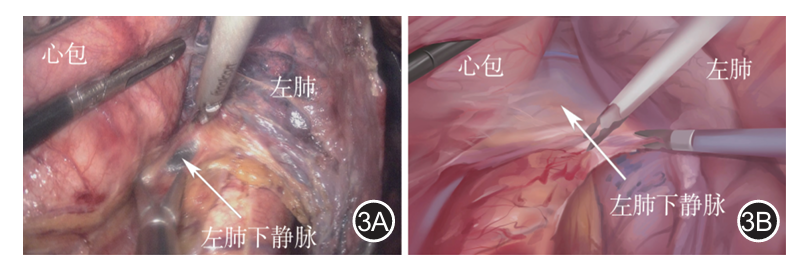
Transabdominal Diaphragmatic Approach with Single-Port Thoracoscopic-Assisted Laparoscopy: Overcoming Siewert Type II Esophagogastric Junction Tumors
Siewert Type II esophagogastric junction adenocarcinoma presents significant surgical challenges and high risks due to the tumor's location in the "special zone" where the esophagus meets the stomach. Traditional open combined abdominal-thoracic surgery is highly invasive and results in slow recovery, often imposing immense physical and psychological stress on patients. Sole reliance on either laparoscopy or thoracoscopy struggles to guarantee both surgical quality, radical tumor resection, and procedural safety.
This year, we have pioneered the single-port thoracoscopic-assisted laparoscopic transabdominal diaphragmatic approach within the province, offering a new minimally invasive treatment option for patients with Siewert Type II tumors. Using this technique, we have successfully performed surgery on multiple patients with high-position esophagogastric junction adenocarcinoma. The procedure involves complete laparoscopic diaphragmatic incision, single-port left thoracic assistance for lower mediastinal lymph node dissection, and intra-thoracic manual esophagojejunostomy. Postoperative outcomes have shown reduced patient pain and faster recovery.
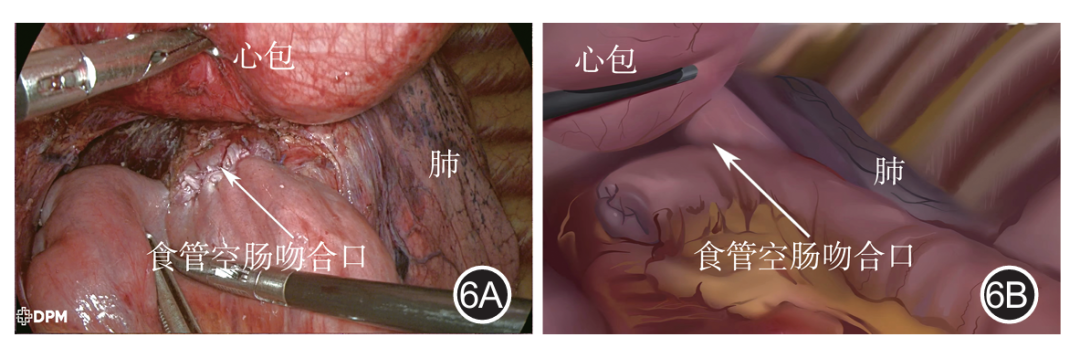
This technique—combining single-port thoracoscopy with laparoscopy—results in minimal trauma and significantly less pain. The laparoscopic transabdominal diaphragmatic approach provides a clear view of the lesion and surrounding structures, enabling both radical tumor resection and thorough lymph node dissection. It maximizes the preservation of normal tissue function, minimizing interference with respiratory and digestive systems. Patients benefit from a quicker recovery, shorter hospital stays, and an earlier return to normal life. This innovative approach perfectly integrates the principles of minimally invasive surgery and precision oncology, offering an optimal treatment solution for patients with high-position esophagogastric junction tumors. It achieves complete eradication of the lesion while significantly enhancing quality of life.
V. Hyperthermic Intraperitoneal Chemotherapy (HIPEC) Revitalizes Vitality:
Directly Targeting Peritoneal Metastasis, Combating Tumors with Hyperthermic Synergy
When gastric cancer progresses to an advanced stage, particularly with the occurrence of peritoneal metastasis, patients and their families often feel the road ahead is daunting. Traditional treatment modalities face limitations in such scenarios, yet medical progress never ceases. In 2025, the Department of Gastric Surgery at Gansu Wuwei Cancer Hospital successfully implemented Hyperthermic Intraperitoneal Chemotherapy (HIPEC), offering tangible new hope to these patients.
What is Hyperthermic Intraperitoneal Chemotherapy (HIPEC)?
HIPEC is an innovative localized treatment that involves continuously and circulatingly perfusing a heated chemotherapy drug solution into the patient's abdominal cavity. It is not merely the sum of "hyperthermia" plus "chemotherapy" but aims to achieve a synergistic attack where "1+1 is far greater than 2."
Its core principle is based on the differential heat tolerance between cancer cells and normal cells. At the precisely controlled therapeutic temperature of 41-43°C, cancer cells become extremely vulnerable as their membrane structures are damaged and DNA repair is inhibited. At this point, high-concentration chemotherapy drugs can act directly on tumor cells and microscopic lesions within the peritoneal cavity, achieving highly effective elimination. Simultaneously, the continuous circulation of the warm fluid acts like a deep "peritoneal cleansing," mechanically flushing away free cancer cells.
Why Should Patients Consider This Option?
For patients with advanced gastric cancer accompanied by peritoneal metastasis, choosing HIPEC is primarily based on the following key advantages:
- Breakthrough Potential in Efficacy: Peritoneal metastasis has been a challenging aspect of gastric cancer treatment, often leading to refractory ascites and intestinal obstruction, with systemic chemotherapy drugs having difficulty penetrating the peritoneal cavity effectively. HIPEC delivers the "weapon" directly to the "core of the battlefield." Multiple authoritative studies (such as GASTRIPEC-I) indicate that combining HIPEC with standard treatment regimens can significantly prolong patients' progression-free survival, increase the opportunity for surgical conversion, and provide a powerful tool for controlling peritoneal lesions and preventing recurrence.
- High Precision and Safety: This technique achieves the effect of "localized intensive attack with systemic toxicity reduction." The drug concentration within the peritoneal cavity can be dozens of times higher than that from intravenous administration, powerfully eliminating tumors, while the amount entering the systemic circulation is minimal, thereby greatly reducing systemic toxic side effects commonly associated with traditional chemotherapy, such as bone marrow suppression and severe nausea and vomiting.
- Relatively Comfortable Treatment Process: During the procedure, patients typically only feel a uniform warmth in the abdomen, with many describing it as "like a deep abdominal heat compress," often experiencing relief from pre-existing abdominal distension. The treatment is conducted under anesthesia or sedation, making the experience smoother.
Our Practice and Commitment
The Department of Gastric Surgery is dedicated to the comprehensive diagnosis and treatment of gastric cancer, staying abreast of technological frontiers. With the introduction of advanced HIPEC equipment at our hospital, the department has systematically implemented this treatment for eligible patients based on domestic and international guidelines and mature experience. We have established a multidisciplinary, refined workflow: perfusion catheters can be accurately placed either during surgical laparoscopic exploration or under ultrasound guidance, ensuring treatment safety and individualization. Building on this, we have developed our own clinical practice insights and established stringent standard operating procedures, striving to provide every patient with standardized, cutting-edge, and compassionate care.


The treatment journey for advanced gastric cancer with peritoneal metastasis remains fraught with challenges. However, the emergence of innovative technologies like Hyperthermic Intraperitoneal Chemotherapy (HIPEC) is continuously expanding the boundaries of life. It represents a more precise and proactive treatment strategy, aimed at helping patients gain more time and quality of life, rekindling hope.
VI. Robotic Surgery: Guiding the Future
Refining the "3+1" Model, Innovating Standards with Precision
In the field of surgical treatment for gastric cancer, radical surgery remains the cornerstone. With the rapid evolution of minimally invasive techniques, surgical approaches have progressed from traditional open surgery, through the laparoscopic era, and entered a new epoch of robot-assisted surgery. Robotic systems, leveraging their exceptional flexibility, precision, and stability, are reshaping the practice of gastric cancer surgery, guiding procedures towards greater minimal invasiveness and intelligence.
In recent years, robotic radical gastrectomy in China has predominantly utilized operational models such as "4+1" or "3+2." Under the leadership of our discipline head, Vice President Nie Peng, our department has long been dedicated to advancing minimally invasive gastric cancer therapy. Starting in 2025, while actively utilizing the domestic Toumai robotic surgical system, we have embarked on in-depth exploration and innovation of surgical models. Moving beyond initial attempts with the "4+1" model and integrating domestic clinical experience with accumulated laparoscopic surgical expertise, the team successfully refined and implemented a new "3+1" model for robotic radical gastrectomy—using three robotic arms assisted by one surgical assistant. This refinement is not merely a numerical adjustment but a deliberate optimization based on efficiency and efficacy. Compared to the "3+2" model, which requires two assistants, the "3+1" model **significantly optimizes human resource allocation while ensuring radical resection and surgical safety. It allows the assistant to provide more focused and efficient support during critical steps, particularly in digestive tract reconstruction. This approach skillfully achieves an ideal balance among the thoroughness of oncological resection, the safety of the surgical procedure, and the functionality required for rapid postoperative patient recovery, embodying the modern surgical principles of "precision, minimally invasive, and enhanced recovery." Initial clinical practice has demonstrated that robotic radical gastrectomy itself offers distinct advantages, including reduced hospital stays, lower complication rates, and notably, more thorough lymph node dissection. The application of the "3+1" model further highlights its core strengths of streamlined workflow and efficient team collaboration, gradually forming a distinctive technical feature of our department in the field of robotic gastric cancer surgery.


Looking ahead, the development of robotic surgery is destined for deeper integration with cutting-edge technologies such as artificial intelligence, machine vision, and precision control. The evolution of surgical systems toward single-port access, miniaturization, enhanced intelligence, and automation represents a clear and established trend. Our department will remain focused on this frontier, actively exploring the integrated application of multiple technologies to drive continuous breakthroughs in robotic gastric cancer surgery, enabling it to truly become a pivotal force transforming the landscape of gastric cancer surgery.
The "3+1" model for robotic radical gastrectomy represents not merely an optimization of technical procedure, but an upgrade in treatment philosophy and team collaboration. It signifies a solid step forward for gastric cancer surgery toward greater precision, efficiency, and patient-centric care, ultimately aiming to deliver tangible benefits to a greater number of patients.
VII. Cloud Live-Streaming Connects the Talented:
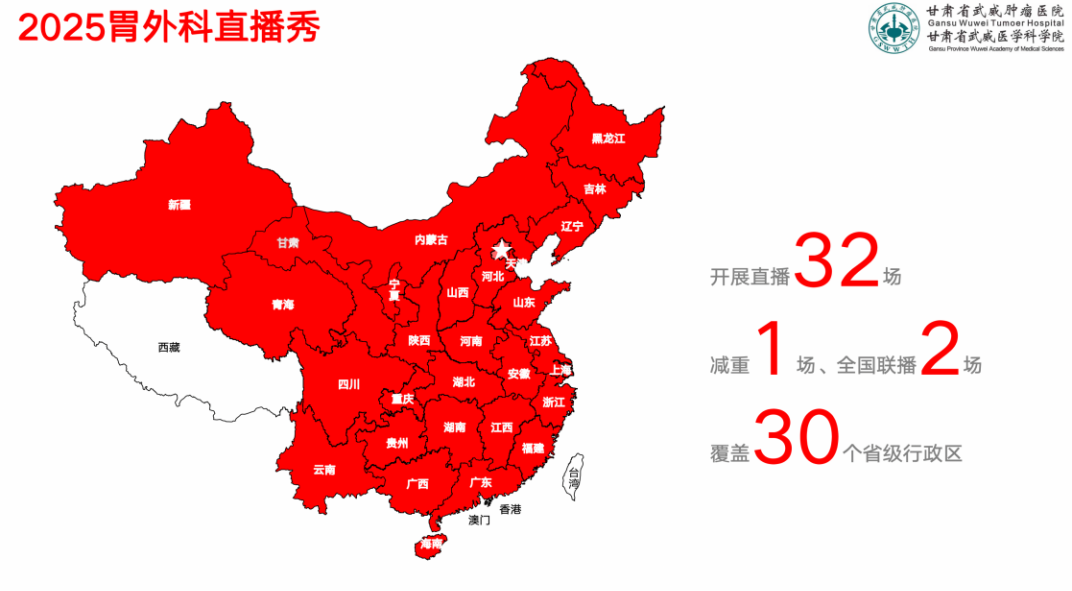
Real-Time Sharing of Surgical Techniques, Exchanging Knowledge Without Borders
Over the past year, our department has made significant progress in the clinical practice of laparoscopic radical gastrectomy and gastric stromal tumor resection. Concurrently, the format of surgical live-streaming has gradually integrated into our technical exchange and demonstration activities. As an efficient and real-time platform for showcasing surgical techniques, live-streaming has not only allowed our team to demonstrate our expertise on national medical platforms but has also created invaluable opportunities for real-time interaction and in-depth discussions with renowned domestic experts, fostering mutual learning and collective advancement.

This year, our department completed 30 live demonstrations of laparoscopic radical gastrectomy, 2 live demonstrations of laparoscopic gastric stromal tumor resection, and participated in 2 national gastric cancer live-streaming week events. The surgeries covered various procedures, including distal gastrectomy, total gastrectomy, and function-preserving gastrectomy. The live streams focused on showcasing key steps such as laparoscopic lymph node dissection, precise vascular dissection, and digestive tract reconstruction (Roux-en-Y anastomosis, fissure technique esophagogastric anastomosis). The cumulative viewership reached over 10,000 peers from 30 provinces and municipalities across China. Each live session featured real-time commentary, effectively promoting cross-regional and multi-level academic exchange and learning.
Successful live-streaming relies on meticulous preoperative evaluation and management, thorough doctor-patient communication and cooperation, and the exceptional technical skill of the primary surgeon. Furthermore, the surgeon's synchronous commentary and insightful analysis during the procedures significantly enhanced the educational value and viewing experience of the broadcasts. Looking ahead, we will continue to uphold a spirit of pursuing excellence. Through higher-quality and more innovative surgical live-streaming activities, we aim to systematically summarize surgical experience, continuously accumulate technical achievements, and courageously scale new heights in medicine.
VIII. Expanding Frontiers in Metabolic and Bariatric Surgery:
Surgery Reshapes Lives, Comprehensive Management Safeguards the Journey
Guided by the "Healthy China" strategy and propelled by the national weight management initiatives, the Department of Gastric Surgery at Gansu Wuwei Cancer Hospital actively established a multidisciplinary team for metabolic and bariatric surgery. We also played a leading role in launching a Comprehensive Weight Management Clinic, providing patients struggling with obesity and related metabolic diseases with scientific, systematic, and personalized diagnosis and treatment plans. Over the past year, we have successfully helped numerous patients regain their health and confidence through surgery.

Metabolic and bariatric surgery (such as sleeve gastrectomy) is a minimally invasive surgical approach. It fundamentally alters the body's weight regulation mechanisms by reducing gastric capacity and modulating gastrointestinal hormones. This approach not only achieves significant and sustained weight loss but also effectively treats or alleviates various obesity-related metabolic diseases, including diabetes, hypertension, and sleep apnea. It is a comprehensive treatment method managed by a specialized multidisciplinary team.
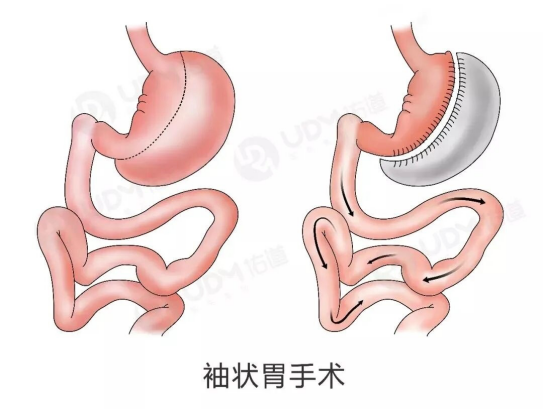
Mr. Zhao, a 24-year-old patient, presented with a body mass index (BMI) as high as 51.6 kg/m², accompanied by multiple comorbidities including hyperlipidemia, hypertension, impaired glucose tolerance, and sleep apnea syndrome, signaling significant health concerns. After comprehensive evaluation and meticulous preparation by our hospital's multidisciplinary team, he underwent a laparoscopic sleeve gastrectomy. Postoperatively, his physical burden was significantly reduced, and various metabolic parameters progressively improved, ushering in a new dawn for his life.
Another patient, Mr. Zhang, aged 40, had a body mass index of 32.6 kg/m² and also suffered from hyperlipidemia and sleep apnea syndrome. Following a sleeve gastrectomy, his weight was effectively controlled, his accompanying symptoms significantly alleviated, and his quality of life substantially improved.
These successful cases highlight our hospital's professional expertise in both the surgical treatment and comprehensive health management of metabolic and bariatric conditions. We focus not only on weight reduction but are also dedicated to comprehensively improving patients' metabolic disorders, preventing long-term complications, and empowering patients to achieve a dual transformation in both physical and mental well-being.
The Metabolic and Bariatric Surgery Team within the Department of Gastric Surgery at Gansu Wuwei Cancer Hospital is committed to safeguarding every patient's health journey, building upon a foundation of exquisite technical skill and connecting through the bond of humanistic care.
IX. Protecting the Critically Ill with Compassion, Safeguarding Health Through Comprehensive Management
76-Day Relay of Life: The Multiple Challenges and Multidimensional Rescue of a Critically Ill Gastric Cancer Patient.
An elderly patient with a gastric body malignancy, a long-term smoker also suffering from obesity and impaired cardiac function, did not embark on a swift path to recovery following laparoscopic gastrectomy. Instead, it marked the beginning of a grueling 76-day life-and-death struggle.
On the third postoperative day, the patient's condition took its first critical turn: sudden chest tightness, shortness of breath, accompanied by atrial fibrillation, followed by a CT scan revealing bilateral lung atelectasis with infection and pleural effusion. In critical condition, the patient was urgently transferred to the ICU for invasive respiratory support. When vital signs temporarily stabilized and the patient returned to the general ward still tethered to multiple treatment lines, an even more formidable series of challenges ensued: multidrug-resistant bacterial infections led to recurrent high fever; imaging suggested a risk of anastomotic leakage; complications included intermuscular venous thrombosis, coupled with difficulties in limb movement and expectoration, leaving the patient temporarily dependent on non-invasive ventilation. The complexity and severity of the condition represented a "cascade of crises"—infections, leakage, thrombosis, and malnutrition intertwined—where a single misstep in any aspect could undo all progress.
Faced with this arduous battle, the Gastric Surgery department rapidly assembled a dedicated rescue team, broke down departmental barriers, and initiated a round-the-clock, multidisciplinary collaborative effort. The medical team adhered to daily multidisciplinary consultations, meticulously adjusted anti-infection strategies based on dynamically changing infection markers, and precisely calculated and optimized every aspect of nutritional support to safeguard the vital functions of the critically ill body. The nursing team established a 24-hour, multi-dimensional monitoring network, with dedicated personnel conducting millimeter-scale monitoring and recording of crucial indicators such as drainage fluid, providing immediate data for decision-making. To tackle the core bottleneck of difficulty expectorating sputum, the team innovatively implemented a triple therapy of "postural drainage + chest percussion + nebulization," simultaneously incorporating acupuncture and bedside rehabilitation training, gradually aiding the patient's recovery from limb weakness to autonomous movement. Concurrent with physical treatment, the medical staff communicated the patient's status daily in plain language and instilled confidence through success stories, stabilizing the emotional fronts of both the patient and the family.
The 76 days and nights of relentless perseverance represented the epitome of teamwork. Ultimately, the infection was controlled, the risk of leakage resolved, the thrombosis subsided, the ventilator was successfully weaned off, and nutrition transitioned smoothly from tube feeding to a normal diet. Upon discharge, the patient was not only out of danger but also gained weight and exhibited robust spirits during subsequent follow-ups. The family specially presented a silk banner inscribed with "Exquisite Medical Skills Alleviate Suffering, Noble Medical Ethics Warm the Heart," expressing their deepest gratitude to the Gastric Surgery medical team.
The success of this rescue was by no means accidental. It profoundly reflects the department's unwavering belief in "never abandoning, never giving up" when managing the small percentage (incidence strictly controlled below 2%) of severe, highly challenging complications that arise even amidst its expertise in handling predominantly (95%) Grade III and IV difficult and complex surgeries. By strengthening teamwork and the multidisciplinary support system, and deeply integrating technical prowess with a "patient-centered" philosophy, the team was able to repeatedly break through bottlenecks at critical moments, upholding the hope of life. This truly demonstrates both the professional depth and humanistic warmth inherent in modern comprehensive gastric cancer treatment.


2025 has been a year of gathering momentum and achieving comprehensive breakthroughs for the Department of Gastric Surgery. We have pursued the ultimate in minimally invasive clinical techniques, striven for source-driven breakthroughs in scientific research, shouldered significant responsibilities in academic leadership, and continuously expanded the scope of our services. Every precise movement of the scalpel, every piece of accumulated research data, and every dynamic exchange of academic ideas have converged into a powerful force propelling our discipline forward and safeguarding patient well-being.
The past year has woven a splendid tapestry of achievements; the coming year beckons us to scale new heights. Looking toward 2026, all colleagues in the Department of Gastric Surgery will steadfastly uphold our founding commitment to "Mastering Medicine with Virtue," maintain the pioneering spirit of "Daring to Lead," and, with more refined skills, warmer care, and a more open-minded approach, continue to write a brilliant new chapter worthy of this era and the sanctity of life on the long journey to conquer gastric cancer!

