Patient, female, 62 years old, pancreatic cancer
Abstract
1. Patient XXX, female, 62 years old, was admitted to the hospital for ‘intermittent epigastric distension and pain for more than half a year, diagnosed with pancreatic cancer for 2 months’. On examination, there was no yellow discolouration of the skin and sclera, no enlargement of superficial lymph nodes, and no abnormalities in the heart, lungs and abdomen.
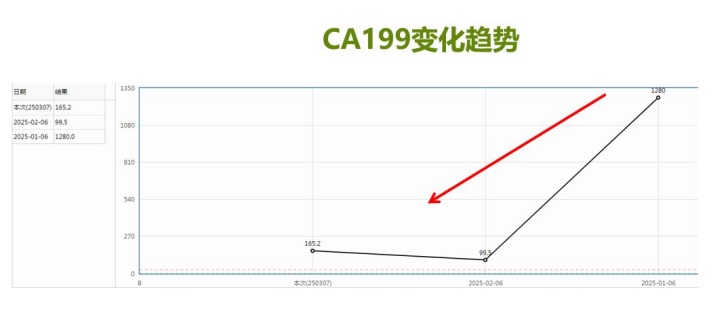
2. Tumour markers of pancreatic cancer: CA-125 97.0U/mL; CA19-9 477.8U/mL; CA24-2 25.1IU/mL; CA-50 362.0IU/mL, all of which were elevated.
3. Biochemical examination: transaminases and bilirubin were elevated. Alanine aminotransferase 83.0 U/L; aspartate aminotransferase 74.5 U/L; direct bilirubin 56.70 μmol/L; total bilirubin 64.20 μmol/L.
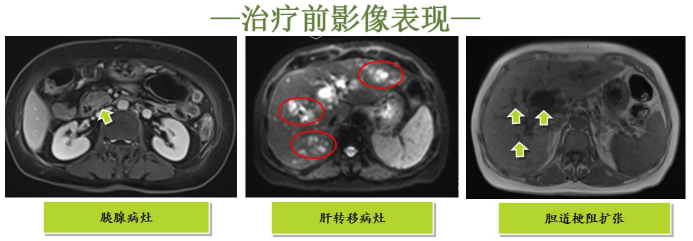
4. Abdominal MRI: the present pancreatic head is full and low-intensified, the lower part of the common bile duct is invaded and truncated, the intra-and extra-hepatic bile ducts and the tail of the pancreatic body are obstructively dilated above the common bile duct, and the intrahepatic diffuse and multiple abnormally intensified nodules are considered as metastasis; the abdominal segment of the para-oesophagus, the intra-abdominal cavity, and the retroperitoneal lymph nodes are displayed, and some of them have enlarged, and metastasis is considered as metastasis.
5. Pancreatic mass puncture histopathology: heterogeneous cells are seen microscopically, suspicious of tumour cells.
Clinical diagnosis
1. malignant tumour of the pancreatic head Extensive liver metastases cT4N2M1 stage IV KPS score: 80;
2. Incomplete common bile duct obstruction;
3. Elevated blood glucose.
Treatment options
1. Placement of a stent in the partially obstructed common bile duct to relieve obstructive jaundice.
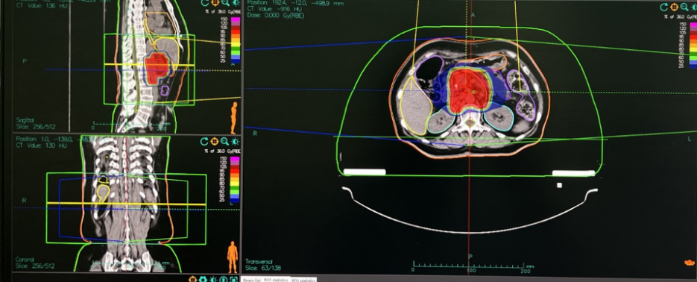
2. Local heavy ion therapy is performed for the primary lesion of pancreatic head cancer, with the prescribed dose of 36Gy (RBE)/12fx and 3.0Gy (RBE)/fx, and the complementary dose of 22.5Gy (RBE)/5f and 4.5Gy (RBE)/f for the retracted field to prevent the tumour from progressing and aggravating the local compression of choledochal ducts and hepatic hilar vessels, and to ensure the smooth circulation of blood and bile to the liver;
3. The systemic treatment plan is: NASOX regimen (Oxaliplatin + Onivyde /Liposomal Irinotecan + S-1 (Tegafur/Gimeracil/Oteracil)+Nimotuzumab
Carbon ion radiotherapy programme
[Efficacy evaluation]: CR
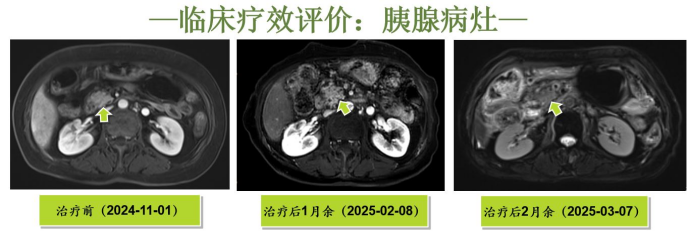
Above is a clinical outcome evaluation: pancreatic lesions, left is before treatment, middle is more than one month after treatment, right is more than two months after treatment.
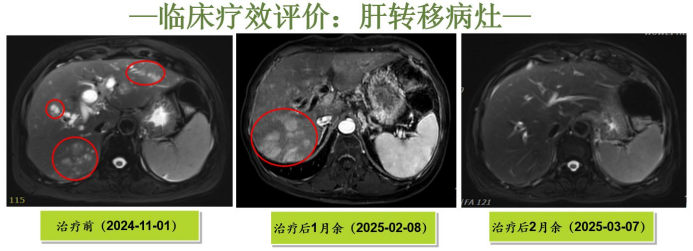
Above is the evaluation of clinical efficacy: liver metastatic lesions, left is before treatment, middle is more than one month after treatment, right is more than two months after treatment.
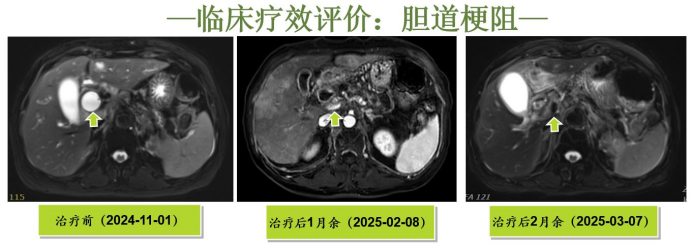
Above is a clinical outcome evaluation: biliary obstruction, left is before treatment, middle is more than one month after treatment, right is more than two months after treatment.
Summary
The patient initially presented with ‘epigastric distension and pain’, accompanied by jaundice, elevated blood glucose and cholestasis, which is in line with the typical manifestations of pancreatic head cancer compressing the common bile duct and impaired pancreatic endocrine function; the imaging showed pancreatic head occupancy and hepatic metastasis, and combined with the pathological diagnosis, it is in line with pancreatic cancer hepatic metastasis (cT4N2M1 stage IV). The patient was already in stage IV at the time of diagnosis, suggesting a poor prognosis and a survival period of 3-6 months in general, but in this case, the patient achieved a very significant therapeutic effect through comprehensive treatment, and the survival period was expected to be significantly prolonged. This patient was treated with a multidisciplinary model, including chemotherapy, targeted therapy, immunotherapy and radiotherapy, reflecting the integrated strategy of ‘systemic therapy + local therapy’ for advanced pancreatic cancer. The patient's biliary obstruction was relieved by carbon ion therapy in combination with systemic therapy, and the metastatic lesions in the pancreas and liver disappeared from the diffusion restriction suggested by MRI DWI, which led to a complete clinical remission.
