The Treatment Journey of Carbon Ion Therapy for Liver Cancer Patients
The Treatment Journey of Carbon Ion Therapy for Liver Cancer Patients: Multidisciplinary Collaboration Opens New Hopes for Life
Patient Basic Information
• Patient XX, male, 50 years old.
• Chief Complaint: A hepatic space-occupying lesion was detected 13 months ago, and hepatocellular carcinoma (HCC) was confirmed 9 months ago.
• Past Medical History: Suffered from hepatitis B for more than 5 years. Regularly took entecavir orally for antiviral treatment, with negative viral replication.
• Admission Date: February 23, 2025
Present Illness
The patient was found to have a hepatic space-occupying lesion during a physical examination on January 5, 2024. It was initially considered as a hepatic hemangioma, approximately 2×3 cm in size. There were no symptoms such as abdominal pain, abdominal distension, nausea, vomiting, poor appetite, or fatigue. No further diagnosis or treatment was carried out. On May 1, 2024, a follow-up examination showed that the maximum diameter of the original hepatic space-occupying lesion increased to 8.3 cm. The patient then visited Peking University Cancer Hospital. A liver biopsy revealed the presence of malignant tumor cells, and hepatocellular carcinoma was suspected. Subsequently, the patient underwent 5 cycles of targeted and immunotherapy with "Tislelizumab 200 mg intravenous drip on day 1 + Lenvatinib 12 mg orally once daily on days 1 - 21, every 21 days". During this period, follow-up evaluations showed that the condition was stable. On November 7, 2024, the patient visited the Chinese Academy of Medical Sciences Cancer Hospital for a pathological consultation, which confirmed hepatocellular carcinoma. Immunohistochemistry showed Ki67 at 20%. Later, the patient participated in a clinical trial of ADC drugs for 4 cycles (details unknown). On December 20, 2024, a chest and abdominal CT scan showed:
1. Multiple nodules and mass shadows in the left lobe of the liver, some of which were fused, with blurred boundaries. The largest one was approximately 6.9×5.9 cm.
2. A filling defect in the left branch of the portal vein, suggesting the formation of a tumor thrombus. The alpha-fetoprotein (AFP) level was 6586 ng/ml. The therapeutic effect was evaluated as stable disease (SD). During the treatment, adverse drug reactions such as hyperglycemia and thrombocytopenia occurred, which were well controlled after symptomatic treatment. For further treatment, the patient came to our hospital. After visiting the outpatient department of our hospital, the patient was admitted to the hospital with a diagnosis of "malignant hepatic tumor". Since the onset of the disease, the patient has been clear-headed, in relatively good spirits, with a good appetite, good sleep, normal bowel and bladder habits, and no significant change in body weight.
Current Diagnosis
• Malignant hepatic tumor (hepatocellular carcinoma, Child-Pugh class A, BCLC stage C, CNLC stage IIIa, cT4N1M0 IVA stage, KPS score 90 points)
• Chronic hepatitis B virus infection
• Liver cirrhosis
• Portal vein tumor thrombus
• Simple renal cyst (left kidney)
• Splenomegaly
Previous Examinations and Diagnosis & Treatment Process
On February 25, 2025, the results of an abdominal MRI showed that it was a follow-up examination for a patient with hepatocellular carcinoma after treatment. Currently, there are multiple abnormally enhanced nodules and masses in the liver, some of which are fused. Please combine with clinical findings and follow-up examinations. There is a filling defect in the lumen of the main trunk and branches of the portal vein, especially in the left branch, suggesting the formation of a thrombus. There is cholecystitis and biliary stasis; splenomegaly; accessory spleen; small cyst in the left kidney; a small amount of fluid around the spleen; several small lymph nodes in the right cardiophrenic angle, abdominal cavity, and retroperitoneum.
On February 27, 2025, the PET/CT showed:
1. The liver lesion underwent a liver biopsy, which suggested hepatocellular carcinoma. The patient underwent multiple cycles of immunotherapy and targeted drug treatment: ① A slightly low-density mass in segment SV of the liver, with unclear boundaries and slightly increased metabolism (slightly higher than the liver background), most likely residual activity of hepatocellular carcinoma after treatment. Please combine with MRI examination. ② Liver cirrhosis and splenomegaly.
2. Sinusitis of the right maxillary sinus; several nonspecific small lymph nodes in the bilateral cervical muscle and soft tissue spaces.
3. A small nodule shadow in the lower lobe of the left lung, with no abnormal metabolism, most likely inflammatory, and follow-up examination is recommended; several small nodules under the pleura of the right lung, with no abnormal metabolism, most likely inflammatory, and follow-up is recommended; arc-shaped ground-glass density shadows under the pleura of both lower lobes of the lungs, with no abnormal metabolism, most likely due to gravitational sedimentation; several small lymph nodes in the mediastinum and bilateral hilar regions, some with slightly increased metabolism, most likely inflammatory.
4. Accessory spleen; increased metabolism in the anal area, most likely inflammatory, possibly hemorrhoids; several small nodule shadows in the mesentery, with no abnormal metabolism, most likely inflammatory, and follow-up examination is recommended.
5. Straightening of the cervical curvature; degenerative changes in the spine.
6. No abnormalities were found in the brain.
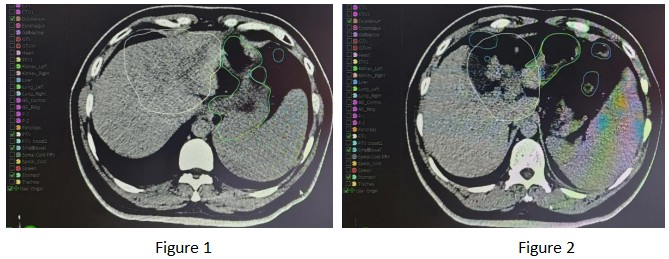
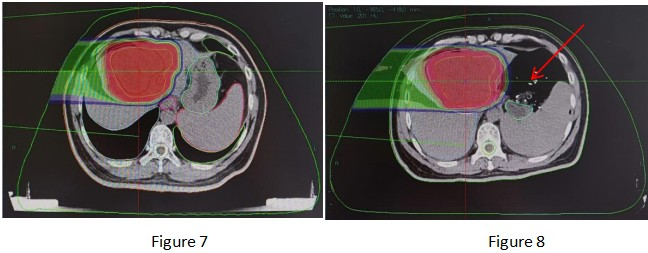
Based on the above imaging examinations, the patient currently has no evidence of distant metastasis, and carbon ion therapy can be performed. On March 4, 2025, the patient underwent radical carbon ion therapy for malignant hepatic tumors. The patient was treated in the prone position. The GTV was delineated based on the hepatic lesions visible on the positioning CT, abdominal MRI, and PET-CT; the ITV was delineated based on the hepatic lesions in all respiratory phases combined with 4D-CT; the GTVm was delineated based on the portal vein tumor thrombus visible on the positioning CT, abdominal MRI, and PET-CT; the CTV was GTV + GTVm + 5 mm, and the CTV was expanded by 5 mm to form the PTV; the PTVboost1 was the PTV avoiding the stomach, small intestine, and duodenum by 8 mm (as shown in Figures 1 and 2).
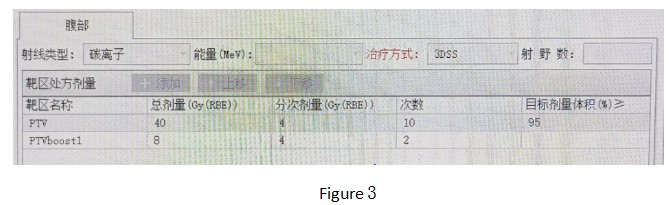
Prescription dose: PTV: 40 Gy (RBE)/9 fractions; PTVboost1: 8 Gy (RBE)/2 fractions (as shown in Figure 3).
Follow-up treatment: After the completion of the initial treatment, due to the non-overlapping areas of PTV and PTVboost in Figure 4 being close to the stomach side and subject to the maximum tolerated doses of the stomach and duodenum, radical treatment doses were not administered.
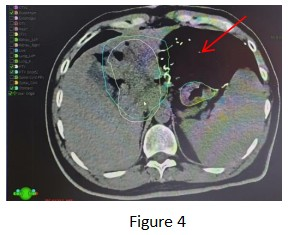
After multidisciplinary consultation in our hospital and with the patient being fully informed and giving consent, we performed a technique pioneered in our hospital, namely exploratory laparotomy + placement of gauze pads to isolate the uninvolved organs (the red arrows in the figure all point to the imaging of the gauze pads).
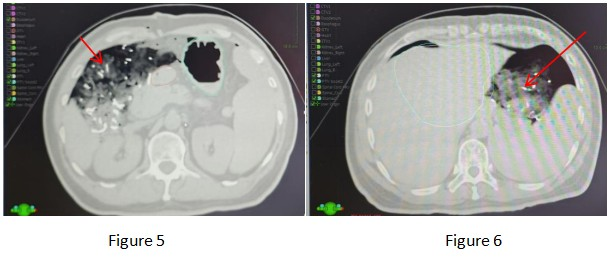
Among them, multiple departments such as the Department of Surgery, the Department of Anesthesiology, the ICU, the Radiotherapy Physics Room, the Radiotherapy Technology Room, the Imaging Department, the Carbon Ion Operation and Maintenance Personnel, and the Ambulance Transfer Staff actively cooperated. After the surgeon evaluated the patient's surgical conditions, an exploratory laparotomy + placement of gauze pads to isolate the stomach and duodenum was performed under general anesthesia. A total of 15 pieces of gauze and one gauze strip were used. The intraoperative bleeding volume was approximately 20 ml, and the operation time was 40 minutes.

operation photos
After regaining consciousness from anesthesia, the patient was transported to the radiotherapy center by ambulance, accompanied by the attending surgeon and anesthesiologist throughout the transport.

A picture of our department assisting the patient from the ambulance to the CT simulation room
The radiotherapy technicians immediately made a immobilization mold, and the Imaging Department conducted a CT simulation scan.

Pictures of mold fixation and CT scanning
After the positioning scan, the patient was transferred to the ICU for close observation, and the vital signs were stable.

Picture of the patient in the ICU
The radiation oncologists in our department actively completed the target volume delineation, taking 1.5 hours to delineate the target area.

Pictures of the physicians in our department delineating the target area
After the target area delineation was completed, the physicist developed a radiotherapy plan for the patient. After the plan was completed, the physicist cooperated with technicians and operation and maintenance personnel to complete the plan verification. Meanwhile, the radiation oncologist completed the pre-treatment setup verification.

Picture of repositioning
After the verification was passed and the errors were eliminated, the patient received a single high-dose radical radiotherapy. The intraoperative radiotherapy dose was 20 Gy (RBE)/1Fx.

Pictures of the treatment process
After the radiotherapy was completed, the patient was transported to the operating room by ambulance. After the gauze pads were removed by the surgeon, the patient was transferred to the ICU for close observation.
Introduction to the Department of Radiation Oncology VI
Specialty Department of Heavy Ion Therapy for Pancreatic Cancer, Department of Abdominal and Pelvic Tumor Treatment
● Department Overview
The Department of Radiation Oncology VI is a specialty department for carbon ion therapy of pancreatic cancer and a department for carbon ion therapy of abdominal and pelvic tumors. It mainly focuses on carbon ion therapy for pancreatic cancer, as well as heavy ion and photon radiotherapy for abdominal and pelvic tumors such as liver cancer, colorectal cancer, and prostate cancer. Since its opening, patients with pancreatic cancer from all over the country have come here attracted by its reputation. It can precisely kill pancreatic cancer cells in patients without pain, surgery, or damage. Dozens of patients with pancreatic cancer from all over the country have been treated successively. The local control rate at 1 year is as high as over 90%, and the median survival time has been increased from the traditional 11 months to 19 months. The clinical efficacy is definite, the patients have a good treatment experience, and the treatment effect has been fully recognized by well-known experts at home and abroad and the vast number of patients.
● Professional Team
All team members graduated from well-known medical colleges in China and have a solid foundation of medical theories and rich clinical practical experience. The department has specially invited experts such as Professor Haofei from Germany, Professor Hirohiko Tsuji from Japan, Professor Yee-Min Jen from the Taiwan region of China, and Professor Jia-Ming Wu to guide the work, conduct consultations on difficult cases, give academic lectures, and conduct ward rounds. The department staff have successively completed further studies and training in many well-known heavy ion and photon treatment centers in China and have rich experience in heavy ion treatment, being able to formulate scientific and reasonable treatment plans for patients.

● Treatment Scope
The department mainly focuses on heavy ion treatment of pancreatic cancer. At the same time, it carries out heavy ion and photon treatment for abdominal and pelvic tumors such as liver cancer, colorectal cancer, and prostate cancer, and can provide patients with professional radiotherapy and personalized comprehensive tumor treatment services.
Introduction to Department Experts:

Chen Weizuo
● Director of the the Department of Radiation Oncology VI, Heavy Ion Center, Gansu Wuwei Cancer Hospital,Deputy Chief Physician
● "Outstanding Young Talent of Longyuan" in Gansu Province
● Director of the Branch of Brachytherapy and Intelligent Radiotherapy of the Chinese Nuclear Society
● Committee Member of the Youth Branch of the Western Radiation Oncology Association
● Committee Member of the Branch of Ion Radiation Therapy of the Chinese Medical Equipment Association
● Committee Member of the IR Youth Committee of CRTOG (Chinese Research Group on Thoracic Oncology) in Radiotherapy and Immunotherapy
● Committee Member of the Youth Committee of the Gastric Cancer/Colorectal Cancer Professional Committee of the Anti-Cancer Association of Gansu Province
● Committee Member of the Radiotherapy Professional Committee of the Wuwei Medical Association
● He presided over 1 project of the Talent Training Program of "Light of the West" of the Chinese Academy of Sciences and 2 talent projects of "Innovation and Entrepreneurship of Young Talents in Longyuan" of the Organization Department of the Gansu Provincial Party Committee.
● He has published 11 SCI papers and 5 papers in Chinese core journals. He has 2 national invention patents and 3 utility model patents. The invention patents won the Gold Award of the "National Invention Exhibition".

Yin Zhaosheng
● Former Director of the Department of Tumor Radiotherapy, Affiliated Hospital of Xiangnan University, Hunan Province
● Standing Committee Member of the Oncology Professional Committee of the Chenzhou Medical Association
● Standing Committee Member of the Anti-Cancer Association of Chenzhou
● Committee Member of the Professional Committee of Tumor Radiotherapy and Radiotherapy Immunotherapy of the Hunan International Medical Exchange and Promotion Association
● Committee Member of the Professional Committee of Clinical Nutrition of the Hunan Medical Education Science and Technology Society
● He has been engaged in clinical tumor treatment for more than 18 years.
● He studied under Professor Yee-Min Jen, the former Chairman of the Radiotherapy Committee of Taiwan Province, China, and Professor Wang Jinzhu, an expert in medical management of Tzu Chi Hospital in Taiwan Province, China.
● Visiting Scholar at Tri-Service General Hospital and Chang Gung Memorial Hospital in Taiwan Province
● He is good at precise tumor radiotherapy, stereotactic radiotherapy, especially the comprehensive treatment of head and neck tumors.
● He has successively studied in advanced studies in major medical centers such as Zhongshan Hospital affiliated to Fudan University in Shanghai, Cancer Hospital affiliated to Sun Yat-sen University in Guangdong Province, Tri-Service General Hospital, and Chang Gung Memorial Hospital in Taiwan Province for many times.
● He has published 4 SCI papers and 2 papers in national core journals and participated in a number of research projects in Hunan Province.

Scan the QR code and follow us.
