Precision Care: Ultrasound Safeguards Dialysis Lifelines by Detecting Fistula Risks
Precision Care: Ultrasound Safeguards Dialysis Lifelines by Detecting Fistula Risks
The latest Chinese Expert Consensus on Vascular Access for Hemodialysis clearly states that regular ultrasound evaluation is a key measure for maintaining fistula function. Under the concept of refined management, ultrasound examination has evolved from a simple imaging tool into a "navigation system" for fistula management.
01 The Fragile Nature of the Lifeline
Vascular access is the lifeline for hemodialysis patients, and arteriovenous fistula is currently the most ideal long-term vascular access. It involves surgically anastomosing an artery with an adjacent superficial vein, arterializing the vein to meet the blood flow required for dialysis. Studies have shown that over 85% of fistula dysfunction is related to vascular stenosis. These stenoses often develop silently without warning. By the time insufficient flow or elevated venous pressure occurs during dialysis, irreversible thrombosis has usually already formed.

02 Precise Insights Beyond Inspection, Palpation, Percussion, and Auscultation
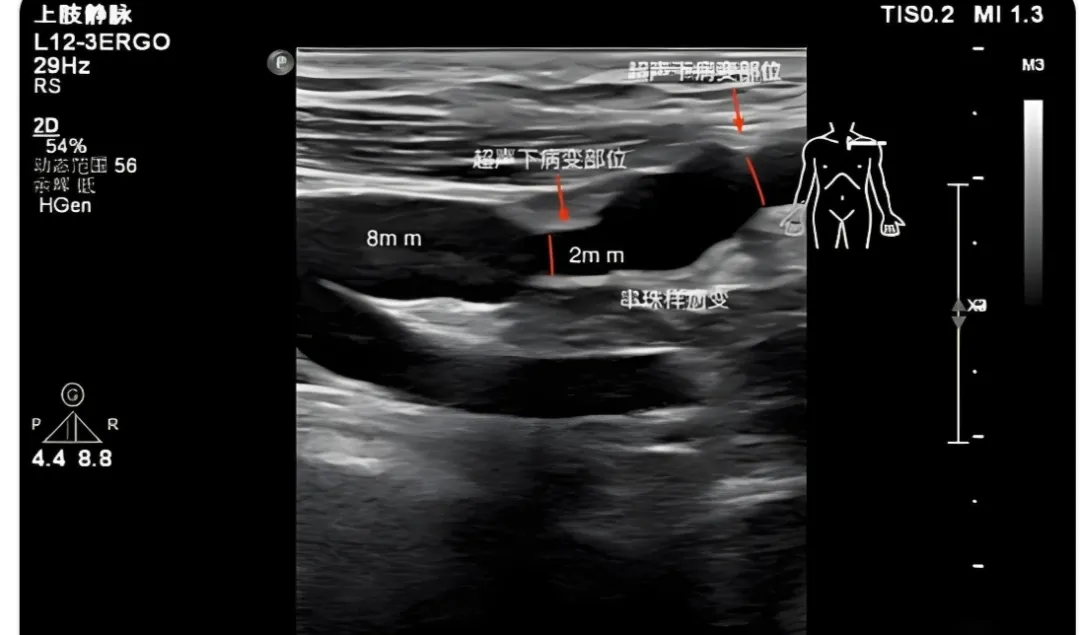
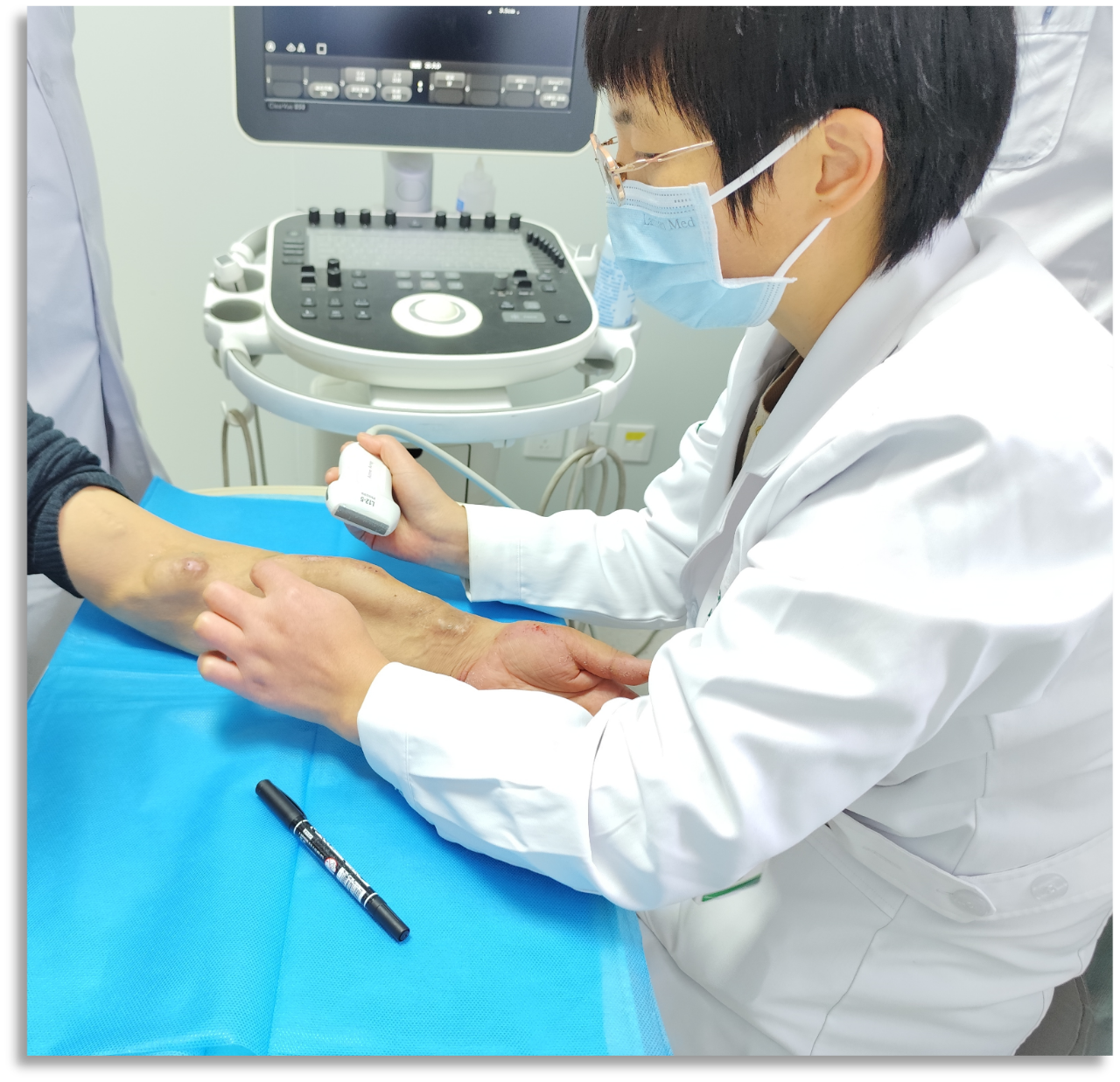
Traditional fistula assessment primarily relies on inspection, palpation, and auscultation. While these methods are simple and easy to perform, they are highly subjective and often only detect problems when the lesion is already quite advanced. In contrast, color Doppler ultrasound can provide objective and precise data, such as vascular internal diameter, blood flow volume, and flow velocity, assisting clinicians in identifying issues at an early stage of disease development. Color Doppler ultrasound not only displays vascular structure but also shows blood flow direction and velocity in real time, while providing hemodynamic parameters. This enables physicians to gain a comprehensive understanding of the fistula's anatomical and functional status, providing a basis for developing personalized management plans.
03 Ultrasound Navigation for the Entire Arteriovenous Fistula Cycle
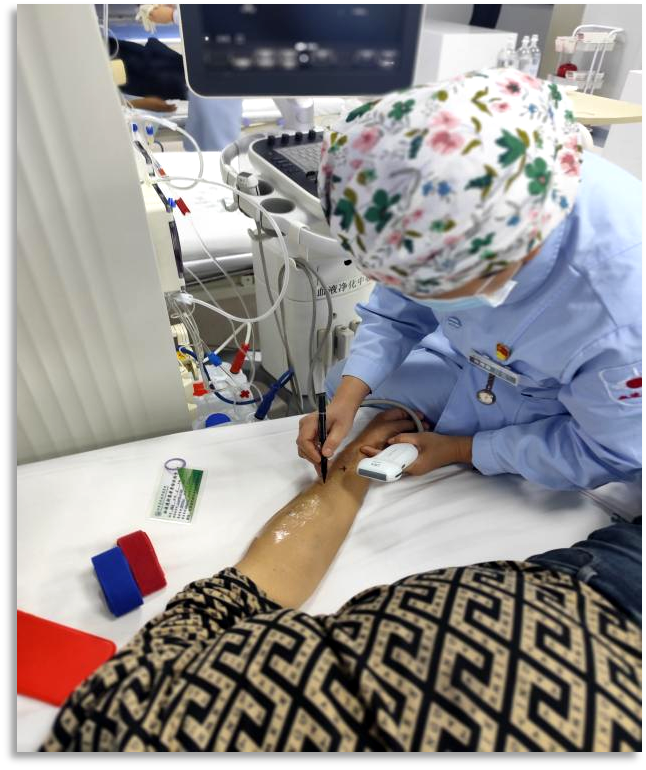
Ultrasound is applied throughout the entire process of fistula management. Preoperatively, it can assess the patient's vascular condition and select the optimal blood vessels and anastomotic site. Studies show that preoperative ultrasound evaluation significantly increases the maturation rate of fistulas, from 60% to over 85%. Postoperatively, ultrasound serves as a crucial tool for assessing fistula maturation. Typically, a mature fistula should have a venous diameter greater than 4-5 mm, a depth from the skin of less than 6 mm, and a blood flow rate exceeding 500 ml/min. For mature fistulas, regular ultrasound monitoring enables early detection of issues. It is recommended to perform a routine ultrasound evaluation every 3-6 months or promptly when clinical abnormalities are observed.

04 Precise Intervention Under Ultrasound Guidance
When ultrasound detects abnormalities in a fistula, physicians can develop precise intervention plans based on the evaluation results. For mild stenosis (<50%), management can involve adjusting the puncture plan or intensifying monitoring. For significant stenosis (>50%), interventional therapy or surgical repair should be considered. Studies have shown that the success rate of percutaneous transluminal angioplasty performed under ultrasound guidance exceeds 90%. Ultrasound is not only used to guide punctures but also to monitor the effectiveness of balloon dilation in real time, assess the degree of residual stenosis, and ensure treatment efficacy.
05 Refined Management of Doctor-Patient Cooperation
Under the framework of refined management, patient self-monitoring is equally important as professional ultrasound evaluation. Patients should learn to check daily for fistula thrill and bruit, observe for abnormalities at puncture sites, and record changes in dialysis parameters. When weakening thrill, altered bruit, or abnormal dialysis parameters are noticed, prompt medical consultation for ultrasound evaluation is essential. Collaboration between doctors and patients is key to achieving long-term patency of the fistula. Regular ultrasound evaluations provide an objective basis for communication between both parties. When patients see their own vascular conditions on ultrasound images, they can more intuitively understand the fistula's status, thereby enhancing treatment compliance.
The thrill in the fistula once again becomes strong and regular, like a river that has regained its vitality, continuing to carry the hope for sustaining life.
