Interventional Therapy Steps In, Pulmonary Artery Thrombosis Trembles Too
Interventional Therapy Steps In, Pulmonary Artery Thrombosis Trembles Too
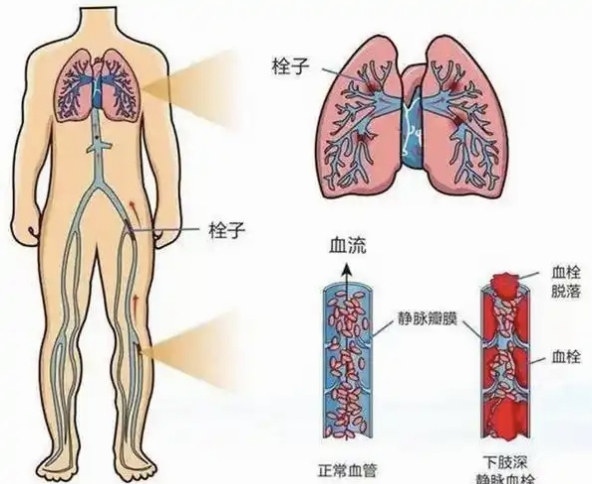
Understanding Pulmonary Embolism: The Silent Deadly Killer
Pulmonary embolism (PE) is a common clinical critical illness. When a blood clot dislodges from the deep veins of the lower limbs and travels with the blood flow to block the pulmonary artery, it triggers a series of life-threatening symptoms. This disease has a sudden onset—mild cases may only present with slight shortness of breath, while severe cases can lead to sudden death within minutes.
Typical Symptom Warnings
● Sudden difficulty breathing (most common symptom)
● Severe chest pain (especially worsens with deep breathing)
● Coughing up blood (occurs in about 30% of patients)
● Unexplained fainting
● Increased heart rate, decreased blood pressure

High-Risk Groups Should Be Vigilant
● Those who are bedridden or sedentary for long periods (e.g., long-distance travel, postoperative recovery)
● Patients who have recently undergone major surgery
● Cancer patients
● Pregnant and postpartum women
● Those with a history of thrombosis or family history
Interventional Thrombectomy: A New Option for Pulmonary Embolism Treatment
Traditional treatment methods have significant limitations: anticoagulant drugs take effect slowly, thrombolytic therapy carries a high risk of bleeding, and surgical procedures are highly invasive. The emergence of interventional pulmonary thrombectomy offers a superior treatment option for patients with pulmonary embolism.
Technical Principle
Doctors perform a femoral vein puncture and, under X-ray guidance, guide a specialized catheter to the site of the pulmonary artery thrombus. Mechanical suction or specialized thrombectomy devices are used to directly remove the thrombus, rapidly restoring pulmonary blood flow.
Main Technical Types
- Catheter suction thrombectomy: Directly aspirates fresh thrombi
- Thrombectomy stent system: Deploys a special stent to capture the thrombus, which is then removed entirely
- Mechanical thrombus fragmentation: Breaks down large thrombi into smaller pieces for removal
- Combined techniques: Utilizes multiple methods based on the patient’s condition
Significant Advantages of Interventional Thrombectomy
- Rapid effectiveness: The procedure is typically completed within 1-2 hours, and patients can immediately feel an improvement in breathing post-surgery. Clinical data show that blood oxygen saturation can quickly increase by 15%-30% after the procedure.
- High safety: Compared to the 20% risk of major bleeding with systemic thrombolytic therapy, interventional treatment has only about a 3%-5% rate of serious bleeding complications.
- Broad indications: Particularly suitable for high-risk pulmonary embolism patients with shock, those with contraindications to thrombolysis, cases where thrombolytic therapy has failed, and some patients with chronic thromboembolic pulmonary hypertension.
- Rapid recovery: Most patients can get out of bed within 1-2 days post-surgery and be discharged in 3-5 days, significantly shortening recovery time.
Real Case Studies
Case 1:
A 79-year-old woman suffered a massive pulmonary embolism after trauma, with blood pressure dropping to 98/52 mmHg and blood oxygen saturation at 85%. Emergency interventional thrombectomy was performed, resulting in an immediate drop in pulmonary artery pressure. The patient was able to sit up and eat the next day.
Case 2:
A 66-year-old woman experienced progressive lower limb swelling for 10 days, followed by sudden chest pain, chest tightness, and shortness of breath for 2 days. She was diagnosed with pulmonary embolism at another hospital but showed poor response to medication, with blood oxygen saturation around 80%. After being admitted to our department, emergency interventional thrombectomy and pulmonary artery thrombolysis were performed, raising her blood oxygen saturation to 98% and significantly relieving her chest pain symptoms.
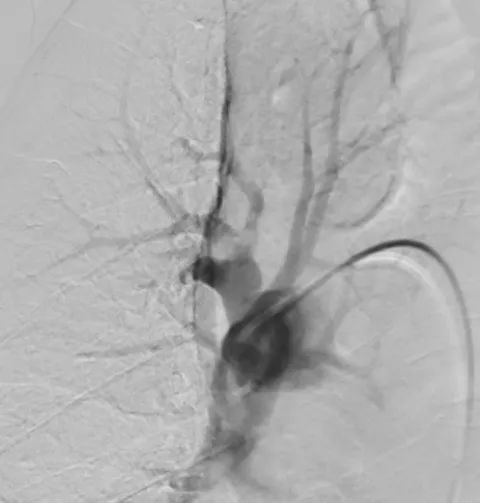
Pre-Surgery
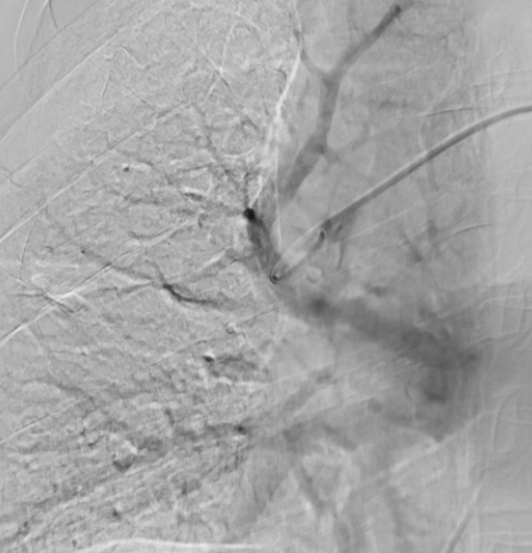
After Thrombus Suction
Prevention Is Better Than Cure
Key Points for Daily Thrombosis Prevention:
a. Avoid sitting for more than 2 hours at a time
b. Regularly move lower limbs during long-distance travel
c. Postoperative patients should get out of bed as early as possible
d. High-risk individuals can wear compression stockings for prevention
Identifying Danger Signals:
If symptoms such as unexplained difficulty breathing or chest pain occur, seek medical attention immediately. Early diagnosis and treatment can significantly improve prognosis.

Director Yang Wangsheng
Key minimally invasive procedures performed in the Cardiology and Interventional Department include:
(I) Heart and Major Vessels:
- Catheter closure for congenital heart disease (atrial septal defect/ventricular septal defect and patent ductus arteriosus); interventional therapy for coronary heart disease (PCI); pacemaker implantation for bradyarrhythmia; radiofrequency ablation for tachyarrhythmia.
- Endovascular exclusion with covered stents for aortic dissection/aneurysm; endovascular exclusion with covered stents for abdominal aortic aneurysm; stent placement for aortic ulcer and aortic intramural hematoma.
(II) Peripheral Vascular Minimally Invasive Procedures:
Balloon angioplasty and stent implantation for lower limb arteriosclerosis obliterans; balloon angioplasty and stent implantation for renal artery stenosis; stent implantation for subclavian artery stenosis; thrombolysis and thrombus suction for deep vein thrombosis of the lower limbs; implantation and removal of inferior vena cava filters; radiofrequency ablation and foam sclerotherapy for lower limb varicose veins; incision thrombectomy and thrombolysis for acute arterial embolism; thrombus suction and catheter-directed thrombolysis for acute pulmonary embolism; embolization for abdominal visceral artery aneurysms.
(III) Tumor Minimally Invasive and Other Minimally Invasive Procedures:
Interventional embolization for major respiratory hemoptysis, major gastrointestinal bleeding, and major gynecological bleeding; interventional therapy for various benign and solid tumors (liver cancer, hepatic hemangioma, uterine fibroids, cervical cancer, soft tissue tumors, etc.); arterial infusion chemotherapy for advanced tumors; interventional diagnosis and treatment for arterial and venous angiomas; implantation and removal of infusion ports for cancer patients.
Address: 1st Floor, Building 1, Heavy Ion Campus, Gansu Wuwei Cancer Hospital
