
Department of Radiation Oncology I, Wuwei Heavy-Ion Center, Wuwei Cancer Hospital, Gansu
(Specializing in Heavy-Ion Treatment for Liver Cancer, Prostate Cancer, and Abdominopelvic Tumors)
Precision Strikes on Tumors, Gentle Protection of Life.
I. Department Overview and Focus
The Department of Radiation Oncology I is a specialized unit for heavy-ion and photon radiotherapy of abdominopelvic tumors. It focuses primarily on treating a wide range of cancers in this region, including liver cancer, cholangiocarcinoma, liver metastases, gastric cancer (pre-operative, post-operative, and advanced non-operative cases), pancreatic cancer, renal cancer, cancers of the ureter and bladder, prostate cancer, and colorectal cancer, using both heavy-ion and photon radiation techniques.
Since its establishment, the department has accepted patients with liver and prostate cancers from across the country. The heavy-ion treatment cycle for liver cancer is short and causes minimal injury to healthy liver tissue. For prostate cancer, precision heavy-ion therapy delivers curative doses while effectively preserving sexual function, ensuring both tumor control and quality of life. The department is recognized for its definitive therapeutic outcomes and positive patient treatment experiences.

II. Talent Team and Academic Structure
The department currently employs 17 staff members, including 8 physicians (1 Chief Physician, 1 Associate Chief Physician, 4 Attending Physicians, and 2 Resident Physicians) and 9 nurses (1 Chief Nurse, 3 Senior Nurses, and 5 Nurses). This constitutes a highly professional, knowledgeable, and dynamic team.
The department places a strong emphasis on talent development. It has appointed Professor Ren Yimin, former Chairman of the Radiotherapy Society in Taiwan, as its technical and academic advisor. Furthermore, department members have participated in exchange and training programs at proton/heavy-ion or photon therapy centers in the United States, Germany, and Japan. They have also pursued advanced studies and academic exchanges at renowned institutions within China, including Sichuan Cancer Hospital, Peking University Cancer Hospital, Sun Yat-sen University Cancer Center, and Zhejiang Cancer Hospital.
These experiences have solidified their foundation in radiation oncology, allowed them to learn advanced techniques, and broadened their perspectives. This enables the team to develop highly personalized and precise treatment plans for each patient.

The department has long retained several internationally renowned experts as consultants, including Professor Jörg Hauffe from the Munich Proton and Heavy Ion Center in Germany, Professor Hirohiko Tsujii, a "pioneer in heavy ion therapy," as well as radiotherapy authorities from Taiwan, China, Professors Yimin Ren and Jiaming Wu. They regularly participate in clinical ward rounds, consultations, and complex case discussions. Additionally, the department has invited Professor Ruitai Fan, Chairman of the Radiotherapy Committee in Henan Province, Professor Zhilong Yu, Chairman of the Radiotherapy Committee in Inner Mongolia, and Professor Shengmin Lan, Chairman of the Radiotherapy Committee in Shanxi Province, to conduct routine ward rounds, contributing to the department's disciplinary development and quality improvement.
The head of the department, Dr. Youguo Ma, has been engaged in radiotherapy for nearly 30 years and has witnessed the growth and expansion of our hospital's radiotherapy department. As a visiting scholar, he conducted exchange studies at the Scripps Proton Center in San Diego, USA, and the National Institute of Radiological Sciences (NIRS) Heavy Ion Treatment Center in Japan. He has also participated in multiple exchange programs at renowned radiotherapy centers across the country, including the Shanghai Proton and Heavy Ion Center, Sichuan Cancer Hospital, and Peking University Cancer Hospital. With extensive clinical experience, he possesses profound expertise in cancer radiotherapy and chemotherapy.

III. Scope of Services and Technical Expertise
The department specializes in heavy ion therapy for liver cancer and prostate cancer, while also providing heavy ion and photon therapy for other abdominal and pelvic tumors, including pancreatic cancer, cholangiocarcinoma, colorectal cancer, gastric cancer, renal cancer, bladder cancer, and secondary malignant liver tumors. It offers patients professional radiotherapy and personalized comprehensive cancer treatment services.
As a specialized department with over 30 years of development, Radiotherapy Department I is a benchmark in the field of precision radiotherapy for cancer in China. The department has established a multi-modal precision radiotherapy system. This system is centered on heavy ion therapy as its core feature and integrates advanced international technologies such as Lattice Radiotherapy (LRT), Stereotactic Radiosurgery (SRS), Volumetric Modulated Arc Therapy (VMAT), Intensity-Modulated Radiotherapy (IMRT), Image-Guided Radiotherapy (IGRT), 3D Conformal Radiotherapy (3D-CRT), interstitial brachytherapy, and surface mold brachytherapy. This approach is combined with comprehensive treatment modalities like surgery, immunotherapy, and targeted drugs. Adhering to the philosophy of "comprehensive treatment and individualized strategies," the department provides patients with standardized, personalized plans involving full-course management. Since its establishment, the department has performed hundreds of heavy ion treatments and cumulatively treated over ten thousand cancer cases with significant efficacy and high patient and family satisfaction.
Department's Specialized Techniques:
1. Heavy Ion Radiotherapy:
•Physical Properties of Carbon Ion Therapy: When charged heavy ions pass through matter, they create a flat, low-dose plateau in the shallow layers. However, as the ions rapidly decelerate at the end of their range, they release their residual energy completely, forming a sharp peak of high ionization density known as the Bragg peak. By adjusting the velocity and intensity of the heavy ions according to the tumor's shape and location, the high-dose region (Bragg peak) can be precisely conformed to match the tumor target volume. This allows for 3D scanning and conformal treatment, maximizing tumor cell destruction while minimally irradiating or sparing surrounding healthy tissue. This characteristic enables heavy ions to minimize radiation dose to adjacent normal tissues, thereby reducing radiotherapy side effects.
•Radiobiological Characteristics of Carbon Ions: Compared to photons, carbon ion beams offer significant biological advantages. Firstly, they have a high Relative Biological Effectiveness (RBE). Carbon ion irradiation causes double-strand breaks in DNA molecules, with about 70% involving complex, less reparable damage to critical sites, leading to efficient tumor cell death. Secondly, the tumor cell kill by carbon ions is largely independent of the cell cycle. Carbon ion therapy not only more readily induces cell cycle arrest in the G2 and M phases but is also effective against tumor cells in the plateau and S phases, which are often resistant to low Linear Energy Transfer (LET) radiation. Its efficacy is almost unaffected by tumor hypoxia, enabling effective destruction of tumor cells. These biological properties of carbon ions overcome the radiobiological limitations of low-LET radiation, demonstrating significant potential for development.
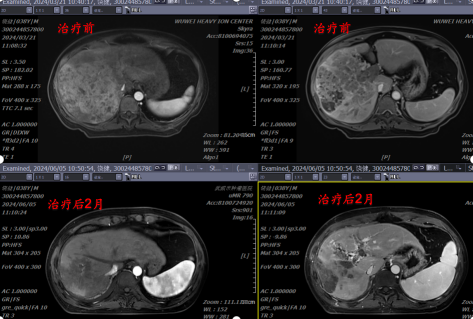
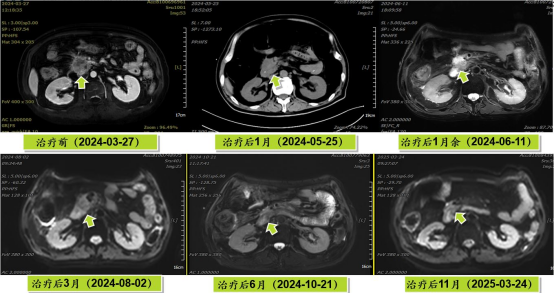
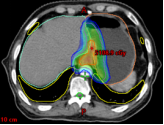
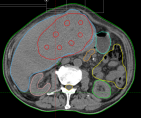
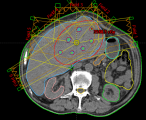
(1) Case Presentation 1: Massive Hepatocellular Carcinoma with Portal Vein Tumor Thrombus
The patient was re-examined over 4 months after initial diagnosis and treatment for liver cancer, presenting with high fever. Abdominal MRI showed an abnormally enhancing lesion in the right hepatic lobe, suggestive of a neoplastic lesion. Low-density shadows were observed filling the right portal vein branch and the main portal vein lumen, indicating thrombus formation.
Pathological Diagnosis: Hepatocellular Carcinoma.
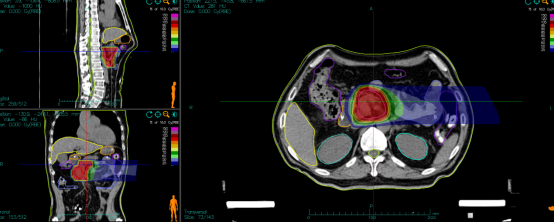
Treatment Plan: Carbon ion radiotherapy, total dose: PTV: 70Gy(RBE)/10 fractions.
Concurrent Therapy: Atezolizumab Injection + Lenvatinib Mesylate Capsules.
Imaging Comparison

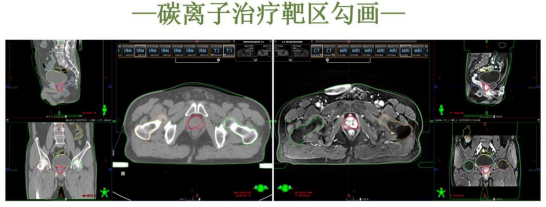
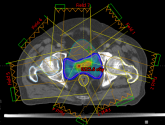
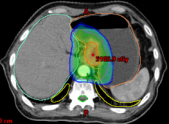
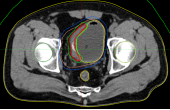
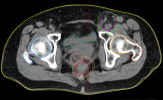
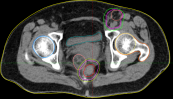
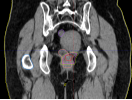
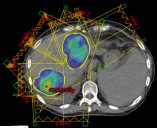
Case Presentation 2: Prostate Cancer
XXX, Male, 64 years old
Chief Complaint: Intermittent perineal pain for 10 months, diagnosed with prostate cancer for 7 months.
Pelvic MRI: An abnormally enhancing mass in the left side of the prostate, highly suggestive of prostate carcinoma, with possible invasion of the left seminal vesicle and a slightly enlarged lymph node in the left pelvis.
Prostate Cancer Markers: TPSA 88.67 ng/ml, FPSA 3.84 ng/ml.
Pathology: (Left prostate biopsy tissue) Prostatic acinar adenocarcinoma, Gleason score 4+3=7; (Right prostate biopsy tissue) Gleason score 3+3=6.
Diagnosis:
1.Malignant neoplasm of prostate, Bilateral, Acinar adenocarcinoma, Gleason score 4+3=7, cT3bN0M0, Stage III.KPS Score: 80.Treatment Plan: Systemic therapy with Goserelin Acetate Sustained-Release Implant 10.8mg subcutaneously and Bicalutamide Capsules 50mg orally once daily; concurrent carbon-ion radiotherapy for prostate cancer, dose: 57.6 Gy (RBE) in 16 fractions.

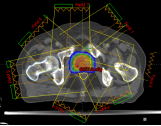
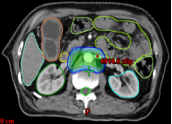
ase Presentation 3: Pancreatic Cancer
The pancreatic adenocarcinoma mass compressed and infiltrated the duodenum, causing duodenal obstruction and an inability to eat normally. The patient required placement of a feeding tube and a gastrointestinal decompression tube. Concurrently, biliary obstruction induced jaundice, necessitating a PTCD drainage tube.
Diagnosis:
1.Malignant Neoplasm of the Pancreatic Head, cT4N0M0, Stage III, KPS Score: 80
2.Incomplete Duodenal Obstruction
3.Obstructive Jaundice
4.Cardiac Arrhythmia, Ventricular Premature Beats
5.Chronic Heart Failure
6.Old Myocardial Infarction
7.Coronary Atherosclerotic Heart Disease
8.Ischemic Cardiomyopathy
Treatment:
Chemotherapy with Gemcitabine + Albumin-bound Paclitaxel was initiated in May 2024 for 4 cycles. Carbon-ion radiotherapy was administered with an initial dose to the PTV of 36 Gy (RBE) in 9 fractions. This was followed by a cone-down boost dose to the PTV of 18 Gy (RBE) in 4 fractions, at 4.5 Gy (RBE) per fraction.
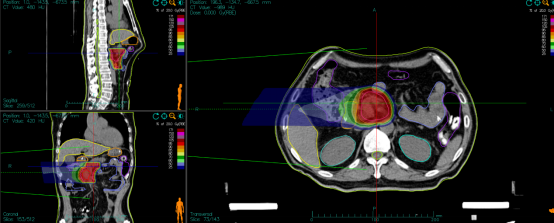
Efficacy Evaluation


2. Application of Photon Radiotherapy Techniques in Abdominal and Pelvic Tumors
This includes techniques such as SABR/SBRT, VMAT, IMRT, IGRT, and 3D-CRT.
SABR/SBRT (Stereotactic Ablative Body Radiotherapy / Stereotactic Body Radiation Therapy) delivers high doses of radiation accurately focused on the tumor in few fractions. It is suitable for early-stage small primary tumors or oligometastases in the abdomen and pelvis, capable of rapidly destroying tumors and significantly shortening the treatment course.
VMAT (Volumetric Modulated Arc Therapy) achieves dynamic dose modulation through continuous rotation of the gantry. It ensures adequate dose to the target while efficiently sparing sensitive abdominal and pelvic organs such as the intestines and bladder.
IMRT (Intensity-Modulated Radiation Therapy) can "tailor" the dose distribution according to the tumor's shape, addressing the challenges posed by irregularly shaped abdominal and pelvic tumors adjacent to critical organs, thereby reducing damage to normal tissues.
IGRT (Image-Guided Radiation Therapy) incorporates real-time imaging verification to accurately correct displacements of abdominal and pelvic organs caused by respiration and peristalsis, ensuring a "precision strike" with radiotherapy.
3D-CRT (3D Conformal Radiation Therapy), as a foundational technique, uses multiple beams to conform the dose distribution to the tumor contour, providing a safe basis for treating complex abdominal and pelvic tumors.
In summary, photon radiotherapy techniques, through "precision focusing, dynamic adaptation, and real-time correction," enhance local control rates for abdominal and pelvic tumors while significantly reducing complications such as gastrointestinal reactions and urinary toxicity, offering patients an effective and safe treatment option.




3. Clinical Research on the Impact of Radiotherapy Intervention on Survival in the Comprehensive Treatment of Inoperable Advanced Gastric Cancer
In the comprehensive treatment of inoperable advanced gastric cancer, radiotherapy has become a core synergistic modality by leveraging its advantages in precise tumor control and symptom palliation. Its application value is mainly demonstrated in three aspects: First, it synergizes with chemotherapy to enhance efficacy. The dose escalation provided by radiotherapy on the local tumor can enhance the sensitivity to chemotherapeutic agents, significantly improving the control rate of the primary lesion and regional lymph nodes, thereby delaying tumor progression. Second, it provides precise symptom relief. For symptoms commonly seen in advanced gastric cancer, such as bleeding, obstruction, and pain, radiotherapy can rapidly reduce tumor size, alleviate gastrointestinal obstruction, control tumor bleeding, and effectively improve the patient's quality of life. Third, it reduces the risk of metastasis. Prophylactic radiotherapy targeting potential micrometastases or oligometastases can decrease the probability of local recurrence and distant metastasis, potentially leading to longer survival for patients. In summary, in the treatment of inoperable advanced gastric cancer, radiotherapy serves as both a "powerful tool for tumor control" and a "key measure for symptom palliation." Through its organic integration with chemotherapy and other modalities, it provides crucial support towards achieving the treatment goals of "prolonging survival and improving quality of life" for patients with advanced disease.
4. Clinical Research on Bladder Preservation with Heavy Ion/Photon Radiotherapy for Inoperable Bladder Cancer
In the bladder-preserving treatment of inoperable bladder cancer, local radiotherapy serves as a core modality to balance "tumor control" and "function preservation." Its application value is highlighted in three key aspects: First, it enables precise bladder preservation. By delivering focused irradiation to the tumor lesion, it effectively eradicates local cancer cells while avoiding the urinary function damage associated with radical cystectomy, thereby fully preserving normal urination function and patient quality of life. Second, it achieves synergistic efficacy enhancement and toxicity reduction. When combined with chemotherapy or immunotherapy, radiotherapy enhances tumor cell kill and improves local control rates. Simultaneously, through precise dose modulation, it reduces the risk of complications such as bladder mucosal injury and intestinal reactions. Third, it offers broad applicability. For patients who are elderly, have multiple comorbidities making them unfit for surgery, or those who refuse radical cystectomy, local radiotherapy serves as a safe and effective alternative, balancing treatment efficacy and patient tolerance.
In summary, local radiotherapy provides an optimal "tumor control + function preservation" strategy for patients with inoperable bladder cancer. It ensures therapeutic effectiveness while significantly enhancing quality of life, establishing itself as a crucial pillar in the bladder-preserving treatment paradigm for bladder cancer.


5. Clinical Research on Sphincter Preservation with Heavy Ion/Photon Radiotherapy for Low-lying Rectal Cancer
In the sphincter-preserving treatment of low-lying rectal cancer, radiotherapy is a key modality that overcomes the limitations of surgery and balances "tumor control" with "anal sphincter preservation." Its application value is demonstrated in three primary aspects: First, it facilitates sphincter-preserving surgery. Neoadjuvant radiotherapy can significantly reduce tumor volume and downstage the cancer, thereby making sphincter-preserving surgery a viable option for low-lying tumors that were initially considered inoperable for preservation. This avoids the impact on quality of life associated with total removal of the anus and the need for a permanent colostomy. Second, it reduces the risk of local recurrence. Through precise irradiation of the tumor and regional lymph nodes, radiotherapy eradicates microscopic disease that may be difficult to remove completely via surgery, thereby significantly improving the local control rate after sphincter-preserving surgery and consolidating the therapeutic outcome. Third, it adapts to diverse clinical scenarios. For patients who are elderly, frail, and unable to tolerate surgery, or for those who refuse a colostomy, radiotherapy combined with chemotherapy can achieve non-surgical radical treatment, effectively controlling tumor progression while preserving anal sphincter function.
In summary, radiotherapy establishes a therapeutic bridge for patients with low-lying rectal cancer, ensuring secure tumor control and viable sphincter preservation. It serves as both a crucial adjunct to sphincter-preserving surgery and a core option for non-surgical management, providing essential support for enhancing both treatment efficacy and patients' quality of life.
6. Clinical Practice, Exploration, and Research of Spatially Fractionated Radiotherapy in Abdominal and Pelvic Tumors
As an innovative precision radiotherapy technique, spatially fractionated radiotherapy demonstrates unique advantages in treating abdominal and pelvic tumors. Its application value focuses on three key aspects: First, it adapts to the anatomical characteristics of the abdomen and pelvis. Through techniques like non-coplanar multi-field irradiation or lattice-like dose distribution, it precisely avoids densely packed sensitive organs such as the intestines, bladder, and spinal cord, effectively addressing the challenge of treating targets adjacent to critical structures in this region. Second, it enhances dose deposition efficiency. By leveraging its characteristic spatial dose fractionation, it creates high-dose foci within the tumor area while reducing the dose to surrounding normal tissues, achieving the therapeutic goal of "high tumor cell kill with low damage to normal tissues." Third, it optimizes treatment for complex lesions. For large, irregularly shaped, or multifocal metastatic tumors in the abdomen and pelvis, it allows flexible spatial dose modulation to address the treatment needs of different lesions simultaneously, improving overall treatment safety and efficacy.
In summary, through its innovative dose distribution patterns, spatially fractionated radiotherapy provides a more precise technical option for treating abdominal and pelvic tumors. It effectively balances treatment efficacy and safety, establishing itself as a significant direction for the development of radiotherapy for complex tumors in this region.

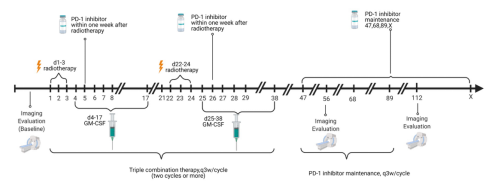
7. Clinical Practice, Exploration, and Research of PRaG Therapy in Heavily Pretreated Advanced Abdominal and Pelvic Tumors
As a precision radiotherapy technique, PRaG (Particle Radiotherapy and Immunotherapy) Therapy provides a crucial treatment option for advanced abdominal and pelvic tumors that have failed multiple lines of therapy. Its clinical value is demonstrated in three key aspects:
First, it breaks through therapeutic bottlenecks. For advanced abdominal and pelvic tumors that have developed resistance to or progressed after multiple lines of treatment (such as chemotherapy and conventional radiotherapy), PRaG Therapy achieves effective tumor kill in resistant lesions through precise dose focusing, thereby overcoming treatment impasses.
Second, it balances efficacy with safety. Leveraging precise targeting and dose modulation, it delivers high doses to tumors while sparing sensitive abdominal and pelvic organs such as the intestines and bladder. This reduces the risk of complications in heavily pretreated patients and enhances treatment tolerance.
Third, it alleviates symptoms and prolongs survival. The therapy can rapidly reduce tumor size, control advanced symptoms like bleeding and pain, and mobilize the body's own anti-tumor immune response. Consequently, it improves patients' quality of life while delaying disease progression, potentially extending survival for those who have exhausted multiple treatment options.
In summary, PRaG Therapy offers a comprehensive solution for heavily pretreated patients with advanced abdominal and pelvic tumors, characterized by "precise tumor control, safe symptom palliation, and activation of innate anti-tumor immunity." It serves as an important technical pillar in the salvage treatment of advanced malignancies.


8. Application and Exploration of 3D Brachytherapy in Rectal Cancer and Interstitial Brachytherapy in Abdominal and Pelvic Tumors
3D brachytherapy and interstitial brachytherapy techniques, leveraging the advantage of precise, localized source placement, provide an important supplementary approach for treating rectal cancer and abdominal/pelvic tumors. Their application value is detailed as follows:
In rectal cancer, 3D brachytherapy delivers a high radiation dose directly to the local tumor area through precise intracavitary or intraluminal source placement. It is particularly suitable for scenarios such as postoperative anastomotic recurrence or residual localized tumor in advanced cases. While effectively protecting surrounding organs like the intestines and bladder, it enhances local tumor control and contributes to the preservation of anal sphincter function.
In abdominal and pelvic tumors, interstitial brachytherapy involves the direct insertion of radioactive sources into the tumor tissue itself, achieving a highly concentrated dose distribution. This technique effectively addresses the challenge of treating complex lesions that are small in volume or adjacent to sensitive organs (e.g., locally advanced cervical or prostate cancer), significantly improving tumor dose coverage while minimizing damage to normal tissues.
In summary, through their approach of "precise, close-range dose delivery," these two techniques provide personalized treatment options for localized rectal cancer and complex abdominal/pelvic tumors, respectively. They constitute vital components of the precision radiotherapy system for malignancies in this anatomical region.






IV. Hardware Facilities
In terms of equipment, the department has introduced several internationally advanced large-scale medical devices, including: a GE Discovery MI PET-CT scanner, a Siemens MAGNETOM Skyra 3.0T superconducting MRI simulation positioning system, a Siemens Somatom Confidence 64-slice simulation CT scanner, a Varian VitalBeam linear accelerator, a Varian Clinac iX linear accelerator, and an Elekta Infinity 4D image-guided linear accelerator. These devices collectively form a comprehensive high-precision radiotherapy platform, providing a solid foundation for clinical treatment.
V. Service Philosophy and Patient Care
The medical team, led by Dr. Youguo Ma, adheres to the core philosophy of "Precisely Targeting Tumors, Gently Guarding Lives." By integrating the technical advantages of heavy ions for "non-invasive ablation" and photons for "precision sculpting," the team directly addresses complex abdominal and pelvic tumors. From intelligent dose optimization to the continuous support of psychological therapists, we have established a closed-loop system of "treatment-rehabilitation-psychological support." Here, cutting-edge radiotherapy technology and humanistic care resonate in harmony, ensuring no one walks their anti-cancer journey alone.

VI. Contact Information and Patient Guide
Inpatient Department Address (Radiotherapy Department I):
First Floor, Building 4, Heavy Ion Center, Wuwei Tumor Hospital (Wuwei Medical Science Academy)
Telephone: 0935-6969631
Vice President Youguo Ma: 13639359095 (also for WeChat)
